Cytomegalovirus (CMV) is a critical opportunistic infection in individuals with advanced HIV infection, particularly those with CD4 counts below 50 cells/µL. CMV primarily manifests as CMV retinitis, the most common cause of blindness in AIDS patients, though it may also present as esophagitis, colitis, pneumonitis, or encephalitis. Effective prevention of CMV disease in advanced HIV patients hinges on immune reconstitution through antiretroviral therapy (ART), targeted screening, and timely prophylaxis or preemptive therapy in select cases.
Understanding CMV Pathogenesis in HIV: A Host-Immune Imbalance
In immunocompetent individuals, CMV remains latent. However, in HIV-infected patients with severe immunosuppression, the virus reactivates and spreads hematogenously, especially when CD4 counts drop below 50 cells/µL.
- CMV Retinitis: Characterized by retinal necrosis, hemorrhages, and cotton-wool spots, leading to irreversible vision loss if untreated.
- Systemic CMV Disease: Involves lungs, gastrointestinal tract, liver, or CNS, though less common than ocular disease.
Risk increases significantly in patients not on ART, those with persistent low CD4+ counts, and individuals with a history of prior opportunistic infections.
Early Diagnosis and Screening: Cornerstone of CMV Prevention
Routine clinical monitoring and targeted screening allow early identification of high-risk patients before symptomatic CMV disease emerges.
Key Components of CMV Risk Assessment in HIV
- CD4 Count Monitoring: Perform every 3 months in advanced HIV stages.
- Ophthalmologic Screening: Fundoscopic exams every 3 months for CD4 <50 cells/µL, even if asymptomatic.
- CMV PCR Testing: Reserved for research or specific diagnostic dilemmas; viremia does not reliably predict CMV end-organ disease in HIV.
Timely diagnosis relies on clinical suspicion and retinal examination rather than viral load alone.
Antiretroviral Therapy: Primary and Most Effective CMV Prevention
Initiating and adhering to combination ART is the most effective strategy to prevent CMV disease in advanced HIV.
ART Mechanism in CMV Prevention
- Immune Reconstitution: Restoration of CD4+ T-cell count (>100 cells/µL) reduces CMV risk dramatically.
- Reduction in Viremia: Lowers activation signals for latent CMV.
- Indirect Benefits: Reduces overall susceptibility to other opportunistic infections, improving clinical resilience.
Initiating ART before CD4+ declines below 100 is critical. However, even in patients with very low counts, immediate ART initiation remains essential.
CMV Prophylaxis in HIV: Current Guidelines and Limitations
Unlike other opportunistic infections (e.g., Pneumocystis or MAC), routine CMV prophylaxis is not recommended in HIV patients due to drug toxicity, cost, and limited efficacy in preventing CMV end-organ disease.
Exceptions Where CMV Prophylaxis May Be Considered
- Patients undergoing ART with delayed immune reconstitution and prior history of CMV disease.
- Those in clinical trials or with particularly aggressive disease patterns.
When used, oral valganciclovir (900 mg once daily) is preferred, though not FDA-approved for CMV prophylaxis in HIV.
Preemptive Therapy: Limited Role in Advanced HIV
Preemptive therapy—initiating antiviral treatment based on rising CMV viremia—is not routinely practiced in HIV management, unlike in transplant recipients.
Reasons for Limited Use
- CMV PCR levels do not correlate well with clinical disease in HIV.
- CMV may remain latent or subclinical even at detectable viral loads.
- Risk of toxicity from ganciclovir or valganciclovir outweighs uncertain benefits without overt disease.
Clinical judgment and direct evidence of tissue involvement remain the mainstay for initiating therapy.
Management of CMV Retinitis in HIV: Immediate and Lifelong Considerations
Early treatment of CMV retinitis is crucial to prevent vision loss and systemic spread.
Standard Treatment Protocol
- Induction Therapy:
- Oral valganciclovir: 900 mg twice daily for 14–21 days
- Alternatives: IV ganciclovir or foscarnet for severe disease or oral intolerance
- Maintenance Therapy:
- 900 mg valganciclovir once daily until CD4+ >100 cells/µL for ≥3 months on ART
Intravitreal Injections
- Ganciclovir (2 mg/0.05 mL) or foscarnet (2.4 mg/0.1 mL) injected directly into the eye for immediate viral control in sight-threatening lesions.
- Often combined with systemic therapy.
Importance of ART Adherence and Resistance Monitoring
ART failure leads to sustained immunosuppression, increasing the risk of CMV and other OIs. It is essential to:
- Monitor HIV viral load every 3–6 months.
- Assess for drug resistance mutations.
- Adjust regimen promptly in case of treatment failure.
Patients with poor adherence or resistance history are at higher CMV risk, necessitating more frequent evaluations.
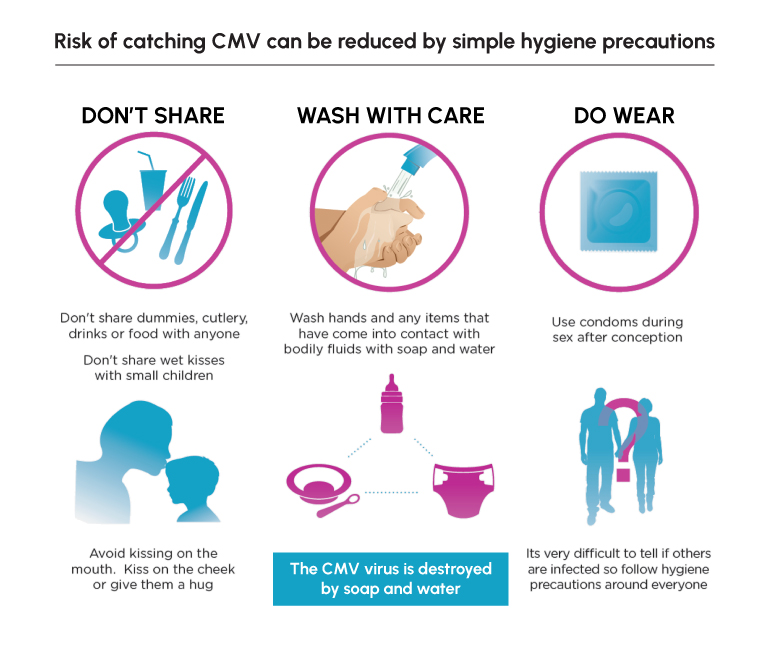
Preventing CMV-Related Blindness: Patient Education and Follow-Up
Patient Counseling Should Include:
- Recognizing early symptoms: floaters, blind spots, blurred vision.
- Emphasizing immediate medical attention for any ocular complaints.
- Understanding the importance of routine eye exams, even when asymptomatic.
- Encouraging adherence to ART and follow-up schedules.
Vision loss from CMV retinitis is irreversible, but preventable with timely action.
Frequently Asked Questions
Should all HIV patients receive CMV prophylaxis?
No. Routine prophylaxis is not recommended. ART-induced immune recovery is more effective and safer for CMV prevention.
What are early symptoms of CMV retinitis?
Floaters, flashes, blind spots, and blurred vision. Asymptomatic retinal lesions may also exist, underscoring the importance of regular fundoscopic exams.
How long should maintenance therapy be continued for CMV retinitis?
Until CD4+ count remains >100 cells/µL for at least 3–6 months with sustained HIV suppression on ART.
Is CMV curable in HIV patients?
Active CMV disease is treatable but not curable. The virus remains latent and may reactivate if immunosuppression returns.
Can CMV occur if CD4 count is above 100?
Rarely. Most cases occur in patients with CD4 <50 cells/µL. Proper ART adherence significantly reduces this risk.
The prevention of CMV disease in advanced HIV patients depends primarily on early initiation and strict adherence to ART, supported by routine eye screening, clinical vigilance, and timely treatment of any signs of CMV retinitis or systemic disease. Although prophylactic antiviral use is limited to specific high-risk scenarios, the integration of consistent immunological monitoring and patient education remains essential. With a well-structured prevention strategy, the incidence of CMV disease—and its associated morbidity—can be drastically reduced in this vulnerable population.