Chemotherapy-induced mucositis is a debilitating inflammatory condition of the mucosal lining of the gastrointestinal tract, most commonly manifesting in the oral cavity. It significantly compromises nutritional intake, causes intense pain, increases infection risk, and often necessitates chemotherapy dose reductions or delays. Given its profound impact on patient outcomes and quality of life, implementing effective preventive measures is a critical component of comprehensive oncology care.
Understanding the Pathogenesis of Chemotherapy-Induced Mucositis
Chemotherapy targets rapidly dividing cells, including the epithelial cells of the gastrointestinal mucosa. This results in mucosal barrier injury, microbial colonization, and inflammatory cascades.
Five-Phase Model of Mucositis Pathogenesis
- Initiation – DNA damage and reactive oxygen species (ROS) generation.
- Upregulation – Activation of transcription factors (e.g., NF-κB).
- Signal Amplification – Cytokine release (TNF-α, IL-6).
- Ulceration – Loss of mucosal integrity, secondary infections.
- Healing – Epithelial regeneration and tissue remodeling.
Risk Factors for Chemotherapy-Induced Mucositis
| Risk Factor | Description |
|---|---|
| Chemotherapy regimen | High-risk drugs include 5-FU, methotrexate, and doxorubicin |
| Hematologic malignancies | Greater mucosal vulnerability due to intense regimens |
| Poor oral hygiene | Increases microbial colonization |
| Nutritional deficiencies | Delay mucosal healing |
| Pediatric or elderly patients | Less mucosal resilience |
| Smoking or alcohol use | Mucosal irritants |
| Concurrent radiation therapy | Exacerbates epithelial damage |
Clinical Approaches to Prevent Chemotherapy-Induced Mucositis
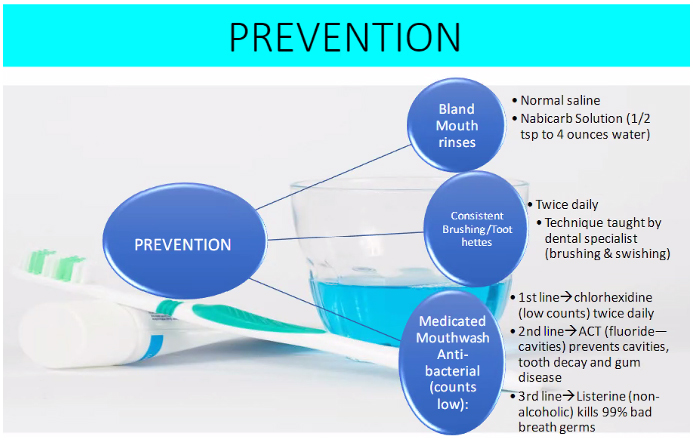
1. Oral Care Protocols and Hygiene Optimization
Effective oral care is foundational in mucositis prevention, reducing microbial load and mechanical trauma.
- Soft-bristled toothbrush used after every meal
- Non-alcoholic mouth rinses (e.g., saline, baking soda)
- Avoidance of irritants such as tobacco, alcohol, and acidic foods
- Routine dental evaluation prior to treatment initiation
2. Cryotherapy for Select Chemotherapy Regimens
Cryotherapy involves cooling the oral mucosa with ice chips during chemotherapy infusion, reducing blood flow and drug exposure.
- Effective for: Bolus 5-fluorouracil and high-dose melphalan
- Protocol: 15–30 minutes before, during, and after infusion
- Mechanism: Vasoconstriction minimizes drug delivery to mucosa
3. Palifermin: Recombinant Human Keratinocyte Growth Factor
Palifermin is FDA-approved for mucositis prevention in hematologic malignancies receiving high-dose chemotherapy and stem cell transplant.
- Dose: 60 mcg/kg/day IV for 3 days before and after chemotherapy
- Mechanism: Stimulates epithelial cell proliferation and healing
- Clinical evidence: Reduces severity and duration of mucositis
Palifermin use is restricted to specific settings due to cost and limited indications.
4. Low-Level Laser Therapy (LLLT)
LLLT promotes cellular regeneration and reduces inflammation through photobiomodulation.
- Wavelengths: 630–660 nm (red light)
- Application sites: Buccal mucosa, tongue, labial mucosa
- Treatment frequency: Daily from start to post-chemotherapy
- Outcome: Significant reduction in mucositis incidence and severity
5. Use of Barrier Protectants and Mucoadhesive Agents
These agents form a protective film over the mucosal surface, minimizing mechanical irritation and microbial invasion.
| Product | Function |
|---|---|
| Gelclair® | Bioadherent gel forming barrier coating |
| Caphosol® | Supersaturated calcium phosphate rinse |
| Episil® | Lipid-based protective oral spray |
6. Antimicrobial and Antiviral Mouthwashes
Though not preventive as standalone agents, antimicrobial rinses may reduce secondary infection risk during mucosal injury.
- Chlorhexidine: Limited preventive efficacy; useful for plaque control
- Benzydamine hydrochloride: Analgesic and anti-inflammatory for oral mucositis prevention in head and neck cancer
7. Glutamine Supplementation
Glutamine is a key nutrient for rapidly dividing mucosal cells. Its supplementation may support mucosal integrity during cytotoxic therapy.
- Form: Oral rinse or powder
- Administration: Begin prior to chemotherapy and continue throughout
- Evidence: Mixed; more effective in parenteral than oral form
Best Practices in Chemotherapy-Induced Mucositis Prophylaxis
- Begin preventive care prior to chemotherapy
- Maintain interdisciplinary coordination between oncology, nursing, and dental teams
- Customize prophylaxis based on chemotherapy type and patient-specific factors
- Educate patients on at-home mucosal care and early symptom recognition
- Utilize evidence-based adjunct therapies when indicated
Frequently Asked Questions
Which chemotherapy drugs are most likely to cause mucositis?
5-Fluorouracil, methotrexate, doxorubicin, and high-dose melphalan are commonly associated with mucositis.
How soon does mucositis occur after chemotherapy?
Symptoms typically begin 5–7 days post-initiation and can persist for up to 3 weeks, depending on severity and treatment duration.
Is mucositis preventable in all patients?
While not entirely preventable, its severity and duration can be significantly reduced with appropriate prophylactic interventions.
Can children receive the same preventive measures?
Yes, but doses and methods must be adjusted for pediatric use, especially for palifermin and laser therapy.
Are natural remedies effective in mucositis prevention?
Some agents like honey and aloe vera have shown modest benefit, but they should not replace standard protocols.
Preventing chemotherapy-induced mucositis demands an integrated, evidence-based approach. From maintaining rigorous oral care routines to deploying pharmacologic and physical modalities such as cryotherapy, palifermin, and low-level laser therapy, clinicians can substantially mitigate mucosal toxicity. Personalized prophylaxis tailored to the chemotherapy regimen and patient profile not only enhances treatment tolerability but also ensures uninterrupted oncologic therapy and improved patient quality of life.