What is Calciphylaxis?
Calciphylaxis, also known as calcific uremic arteriolopathy (CUA), is a rare yet severe condition characterized by progressive calcification of small- and medium-sized blood vessels, leading to ischemic necrosis of the skin and subcutaneous tissues. This condition predominantly affects patients with end-stage renal disease (ESRD) undergoing dialysis, though it can also occur in individuals without kidney disease.
Symptoms of Calciphylaxis
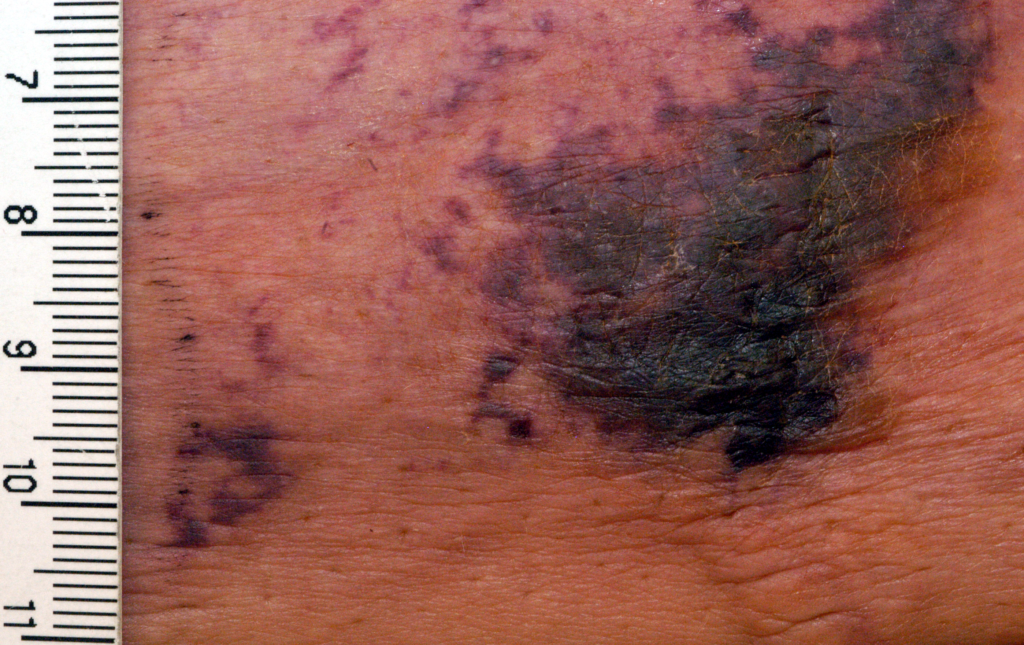
The clinical presentation of calciphylaxis is both alarming and distressing. Key symptoms include:
- Painful Skin Lesions: These lesions are often black, necrotic ulcers surrounded by purplish discoloration.
- Severe Pain: Persistent and severe pain is common, typically localized to the areas affected by skin ulcers.
- Edema and Erythema: Swelling and redness in the affected areas.
- High Risk of Infection: Due to open ulcers, patients are at increased risk of secondary infections, including sepsis.
The condition frequently affects the lower extremities, abdomen, and buttocks, but it can occur anywhere on the body.
Causes and Risk Factors
Calciphylaxis is complex, with multiple contributing factors. The main causes and risk factors include:
- Chronic Kidney Disease (CKD): Most patients with calciphylaxis have ESRD and are on dialysis.
- Dysregulated Calcium-Phosphate Metabolism: Elevated serum calcium and phosphate levels contribute to vascular calcification.
- Medications: Use of warfarin, calcium-based phosphate binders, or vitamin D analogs.
- Hyperparathyroidism: Overactive parathyroid glands exacerbate calcium-phosphate imbalance.
- Obesity and Diabetes: These conditions increase susceptibility.
- Other Risk Factors: Female sex, hypoalbuminemia, and prior history of vascular disease.
Pathophysiology
Calciphylaxis arises from a complex interplay of metabolic and vascular abnormalities:
- Vascular Calcification: Deposition of calcium and phosphate crystals in vessel walls.
- Endothelial Dysfunction: Damage to the endothelial lining due to inflammation and oxidative stress.
- Prothrombotic State: Enhanced clotting activity exacerbates ischemia and tissue necrosis.
Diagnosis of Calciphylaxis
Diagnosing calciphylaxis requires a combination of clinical evaluation, imaging studies, and biopsy:
- Clinical Assessment: Identification of characteristic painful skin ulcers and risk factors.
- Imaging: Techniques like X-rays or CT scans reveal vascular calcifications.
- Biopsy: Skin and subcutaneous tissue biopsy confirms calcification, thrombosis, and necrosis.
Treatment Options
Calciphylaxis treatment focuses on halting disease progression, managing symptoms, and addressing underlying causes:
1. Wound Care
- Regular dressing changes using antimicrobial and moisture-retentive materials.
- Management of secondary infections with targeted antibiotics.
2. Pharmacological Interventions
- Sodium Thiosulfate: Reduces vascular calcification and provides analgesia.
- Cinacalcet: Used to manage secondary hyperparathyroidism.
- Bisphosphonates: Reduce calcium-phosphate precipitation.
3. Surgical Interventions
- Parathyroidectomy: Indicated for refractory hyperparathyroidism.
- Debridement: Removal of necrotic tissue to prevent infection spread.
4. Dialysis Optimization
- Modifying dialysis regimens to improve calcium-phosphate balance.
5. Lifestyle Modifications
- Nutritional counseling to reduce dietary phosphorus and maintain adequate protein intake.
- Weight management and blood glucose control in diabetic patients.
Prognosis
Calciphylaxis has a poor prognosis, with high morbidity and mortality rates, particularly due to sepsis. Early recognition and aggressive treatment are critical to improving outcomes.
Preventive Measures
- Close monitoring of calcium-phosphate levels in high-risk individuals.
- Avoidance of medications known to exacerbate the condition, such as warfarin.
- Proactive management of risk factors, including diabetes and obesity.