Unstable angina represents a critical manifestation of acute coronary syndrome (ACS), characterized by new or worsening chest pain at rest or minimal exertion, without myocardial necrosis. Preventing cardiac ischemia in this context is essential to avert myocardial infarction, minimize morbidity, and improve long-term cardiovascular outcomes. This article outlines evidence-based, multidimensional strategies for the effective prevention of cardiac ischemia in patients presenting with unstable angina.
Understanding the Pathophysiology of Unstable Angina and Cardiac Ischemia
Mechanisms of Ischemia
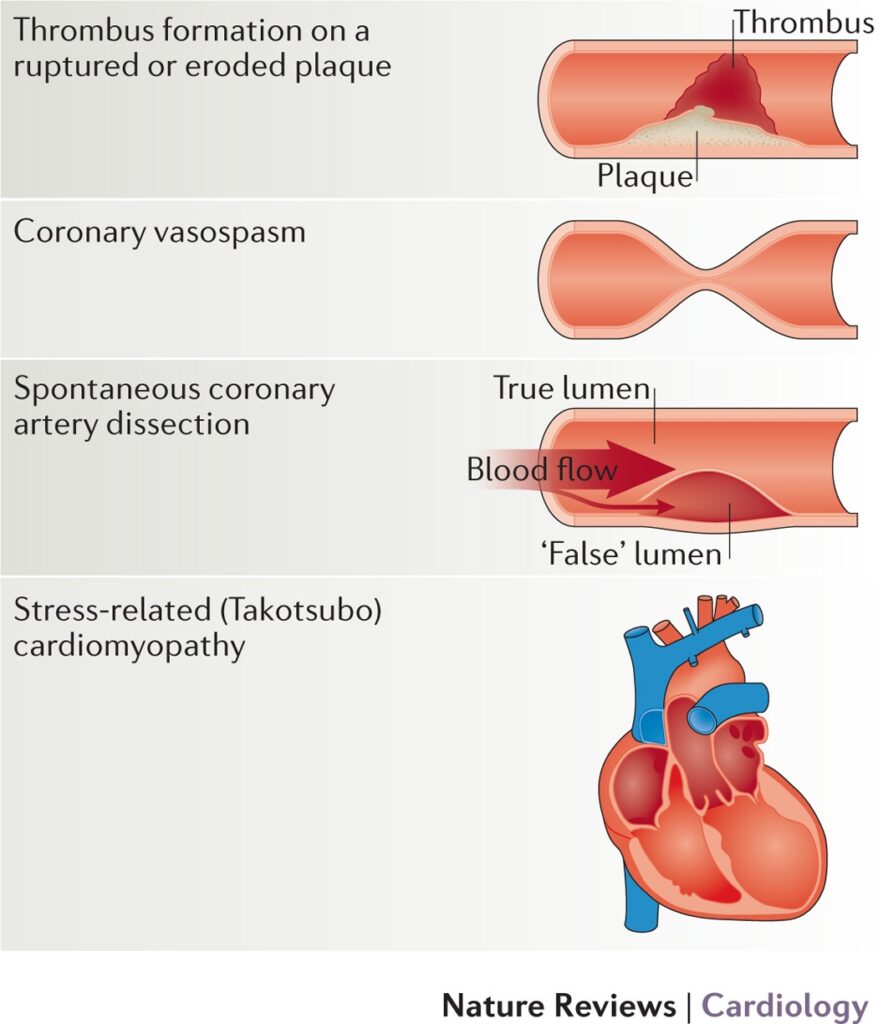
Unstable angina results from an imbalance between myocardial oxygen demand and supply, most commonly triggered by:
- Plaque rupture and thrombosis in coronary arteries
- Endothelial dysfunction
- Vasospasm and microvascular disease
- Dynamic obstruction due to platelet aggregation
This ischemia occurs without detectable myocardial injury markers but signals an impending infarction if not addressed promptly.
Initial Risk Stratification and Monitoring
Risk Assessment Tools
Early identification of high-risk patients enables targeted preventive intervention. Widely used risk stratification tools include:
- TIMI Risk Score (Thrombolysis in Myocardial Infarction)
- GRACE Score (Global Registry of Acute Coronary Events)
These tools consider age, ECG changes, biomarker levels, prior coronary artery disease, and hemodynamic status.
Anti-Ischemic Pharmacologic Therapy
Nitrates
Short-acting and long-acting nitrates reduce myocardial oxygen demand by venodilation and coronary vasodilation. They remain a mainstay for immediate symptom relief.
- Nitroglycerin (sublingual or IV)
- Isosorbide mononitrate/dinitrate (long-term prophylaxis)
Beta-Blockers
Beta-adrenergic blockade decreases heart rate, myocardial contractility, and systemic blood pressure, effectively reducing oxygen consumption.
- Metoprolol, Atenolol, or Bisoprolol preferred in the absence of contraindications
- Cautious use in bradycardia, hypotension, or heart block
Calcium Channel Blockers
In patients intolerant to beta-blockers or with persistent ischemia:
- Non-dihydropyridines (Verapamil, Diltiazem) reduce HR and contractility
- Dihydropyridines (Amlodipine) used in vasospastic angina or hypertension
Ranolazine
An anti-anginal agent used for refractory angina unresponsive to conventional therapy, particularly in patients with chronic ischemic symptoms.
Antiplatelet and Antithrombotic Therapy
Dual Antiplatelet Therapy (DAPT)
Essential in preventing platelet aggregation and thrombus formation.
- Aspirin: Irreversible COX-1 inhibitor administered immediately
- P2Y12 Inhibitors: Clopidogrel, Ticagrelor, or Prasugrel added for synergistic inhibition
Anticoagulants
Unfractionated Heparin (UFH) or Low Molecular Weight Heparin (LMWH) are used during hospitalization to reduce clot propagation.
- Enoxaparin is preferred for its predictable pharmacokinetics
- Bivalirudin or Fondaparinux as alternatives in specific scenarios
Lipid Management and Statin Therapy
High-intensity statin therapy not only lowers LDL-C but also stabilizes vulnerable plaques, reducing the risk of recurrent ischemic events.
- Atorvastatin 40–80 mg or Rosuvastatin 20–40 mg recommended
- Initiated regardless of baseline cholesterol levels in unstable angina
Lifestyle and Risk Factor Modification
Smoking Cessation
Eliminating tobacco use dramatically reduces endothelial dysfunction and inflammation, lowering ischemic risk.
Blood Pressure and Glycemic Control
- Target BP: <130/80 mmHg for most patients
- HbA1c Target: <7% in diabetics to reduce vascular complications
Weight Management and Exercise
- Structured cardiac rehabilitation programs improve exercise tolerance and reduce recurrent ischemic episodes
- Encourage BMI <25 kg/m² with dietary modification and aerobic activity
Early Invasive Strategies and Revascularization
Coronary Angiography
Recommended within 24–72 hours in high-risk patients or those with ongoing ischemia, elevated biomarkers, or ECG changes.
Percutaneous Coronary Intervention (PCI)
- Balloon angioplasty and stent placement restore coronary perfusion
- Drug-eluting stents preferred to reduce restenosis risk
- Post-PCI DAPT essential for stent thrombosis prevention
Coronary Artery Bypass Grafting (CABG)
Considered for multi-vessel disease, left main coronary artery stenosis, or when PCI is not feasible or effective.
Long-Term Medical Therapy Post-Acute Management
Maintenance Therapy
- Aspirin indefinitely
- Beta-blockers long-term, especially post-MI or in LV dysfunction
- ACE inhibitors or ARBs for hypertension, LV dysfunction, or diabetes
- Statins for secondary prevention
Routine follow-up and adherence monitoring are critical to prevent recurrent events.
Emerging Therapies and Future Directions
PCSK9 Inhibitors
Used in patients with persistently elevated LDL-C despite statin therapy. Significantly reduce cardiovascular events.
Inflammatory Modulation
- Colchicine and IL-1 inhibitors show promise in reducing vascular inflammation, a key driver of plaque rupture.
Precision Medicine
- Genotype-guided antiplatelet therapy
- AI-driven risk stratification and management algorithms
Frequently Asked Questions
What is the main goal in treating unstable angina?
The primary objective is to prevent progression to myocardial infarction by reducing myocardial oxygen demand, inhibiting thrombus formation, and restoring coronary blood flow.
Which medications are essential in unstable angina management?
Aspirin, P2Y12 inhibitors, nitrates, beta-blockers, statins, and anticoagulants form the foundation of therapy.
Is PCI necessary for all patients with unstable angina?
Not all patients require invasive procedures. Risk stratification determines whether conservative medical therapy or revascularization is appropriate.
Can cardiac ischemia be prevented without surgery?
Yes, many cases are managed successfully with pharmacologic therapy, lifestyle changes, and vigilant monitoring.
How soon should unstable angina be treated?
Immediate medical evaluation and intervention are crucial to prevent irreversible myocardial injury and complications.