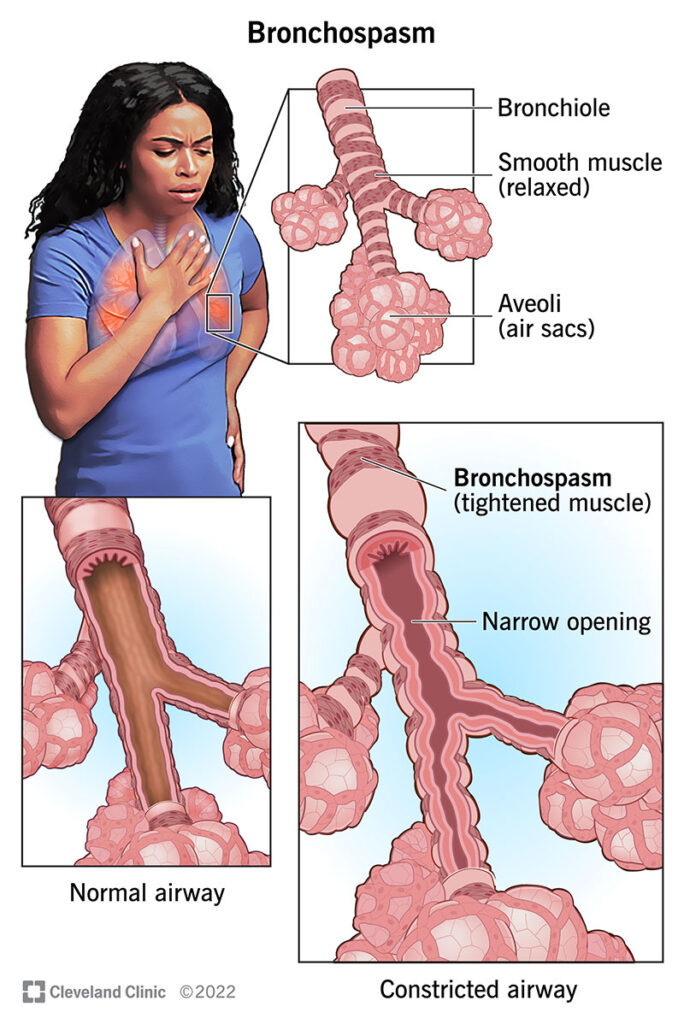
Chronic bronchitis, a form of chronic obstructive pulmonary disease (COPD), is frequently complicated by bronchospasm—an acute, reversible narrowing of the airways due to smooth muscle contraction. Preventing bronchospasm in patients with chronic bronchitis requires a multifaceted, preventive care approach targeting inflammation, airway reactivity, mucus production, and environmental exposure.
Understanding the Interplay Between Chronic Bronchitis and Bronchospasm
Chronic bronchitis is characterized by persistent cough and sputum production for at least three months over two consecutive years. When bronchospasm occurs, it introduces an element of airflow obstruction that is often acute and reversible, compounding the chronic airway inflammation.
Pathophysiology of Bronchospasm in Chronic Bronchitis
- Airway hyperresponsiveness triggered by allergens, pollutants, or infections
- Smooth muscle constriction narrowing the bronchial passages
- Excess mucus production obstructing airflow
- Inflammatory cytokines amplifying the bronchospastic response
Understanding these mechanisms allows us to develop targeted preventive strategies.
Pharmacologic Prevention of Bronchospasm in Chronic Bronchitis Patients
Inhaled Bronchodilators: The First Line of Defense
Short-acting beta-agonists (SABAs) such as albuterol are used for acute relief but can also be part of a preventive regimen when administered before exposure to known triggers.
Long-acting beta-agonists (LABAs) like salmeterol and formoterol maintain bronchodilation and reduce the frequency of exacerbations and bronchospasm episodes.
Anticholinergics, including ipratropium (short-acting) and tiotropium (long-acting), block muscarinic receptors and decrease smooth muscle tone in the airways, providing sustained protection against bronchospasm.
Inhaled Corticosteroids (ICS)
ICS such as fluticasone or budesonide reduce airway inflammation and mucus production, thus lowering bronchial hyperresponsiveness. ICS are particularly effective when combined with LABAs.
Methylxanthines
Agents like theophylline are used less commonly due to side effects but can be beneficial in patients with persistent symptoms not controlled by inhalers alone.
Mucolytics and Airway Clearance Therapies
Reducing mucus obstruction is critical for preventing bronchospasm in chronic bronchitis patients.
- N-acetylcysteine (NAC): Breaks down mucus viscosity
- Carbocysteine: Enhances mucus clearance
- Airway clearance devices (e.g., oscillating PEP devices) support daily sputum mobilization
Regular use of mucolytics can prevent mucus plugging, a key contributor to bronchospasm.
Pulmonary Rehabilitation: Enhancing Respiratory Function and Control
Pulmonary rehabilitation programs, which include supervised exercise training, breathing techniques, and patient education, significantly reduce the risk of bronchospastic episodes.
Key Components
- Pursed-lip breathing and diaphragmatic breathing to reduce airway resistance
- Aerobic conditioning to improve ventilatory efficiency
- Chest physiotherapy to aid in mucus mobilization
- Psychological support to reduce anxiety-induced bronchospasm
Environmental and Allergen Avoidance
Smoking Cessation
Eliminating tobacco smoke exposure is the most effective preventive intervention. Smoking directly increases bronchial inflammation, mucus production, and airway reactivity.
Air Quality Control
- Use of HEPA filters and air purifiers
- Avoidance of dust mites, pet dander, and mold spores
- Limiting outdoor activity during high pollution or pollen index days
Occupational Hazards
Patients should avoid or use protective gear in environments with chemical fumes, dust, or gaseous irritants.
Immunization and Infection Prevention
Respiratory infections are potent triggers of bronchospasm and must be proactively prevented.
Recommended Vaccinations
- Annual influenza vaccine
- Pneumococcal vaccine (PCV20 or PPSV23)
- COVID-19 vaccine boosters as per guidelines
Early Antimicrobial Intervention
Prompt treatment of bacterial or viral respiratory infections with appropriate antibiotics or antivirals helps mitigate inflammation and prevent secondary bronchospasm.
Nutritional Optimization and Hydration
Proper nutrition supports immune function and muscle strength, including respiratory muscles.
- High-protein, low-sodium diet to reduce fluid retention and inflammation
- Adequate hydration helps thin mucus and improves clearance
- Supplementation with omega-3 fatty acids and antioxidants may offer additional anti-inflammatory benefits
Long-Term Monitoring and Follow-Up Care
Consistent follow-up is essential to evaluate symptom progression, adjust therapies, and reinforce preventive practices.
Routine Assessments
- Spirometry to assess airflow limitation
- Symptom scoring tools like CAT or mMRC
- Oxygen saturation monitoring for hypoxia detection
Exacerbation Action Plan
Patients should have a written bronchospasm action plan, outlining:
- When to use rescue inhalers
- When to start corticosteroids or antibiotics
- When to seek emergency care
Effective prevention of bronchospasm in patients with chronic bronchitis hinges on a multidisciplinary approach that integrates pharmacotherapy, environmental control, respiratory rehabilitation, and patient education. By targeting the underlying inflammation and minimizing exposure to triggers, we can significantly reduce the frequency and severity of bronchospastic episodes, thereby improving quality of life and long-term pulmonary outcomes.

