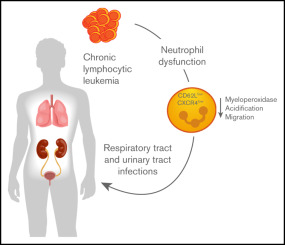
Chronic Lymphocytic Leukemia (CLL) is a hematologic malignancy marked by the accumulation of dysfunctional B lymphocytes. A major cause of morbidity and mortality in patients with CLL is recurrent and severe bacterial infections. Due to inherent immune dysfunction and treatment-induced immunosuppression, infection prevention becomes a cornerstone of comprehensive CLL care.
Understanding Infection Susceptibility in CLL Patients
Patients with CLL exhibit both humoral and cellular immune deficits, which compromise their ability to mount an effective response to pathogens. This vulnerability is amplified during chemotherapy or targeted therapies, particularly with agents such as anti-CD20 monoclonal antibodies and BTK inhibitors.
Key Immunological Deficits
- Hypogammaglobulinemia: Reduced levels of IgG, IgA, and IgM impair opsonization and bacterial clearance.
- T-cell dysfunction: Impaired CD4+ and CD8+ responses limit intracellular pathogen control.
- Neutropenia: Often treatment-induced, it increases risk of gram-negative and opportunistic infections.
Risk Stratification and Surveillance for Infection
A structured approach to infection risk stratification ensures early identification of patients who require preventive interventions.
Infection Risk Categories
| Risk Level | Features |
|---|---|
| Low | Early-stage CLL, no prior infections, normal IgG |
| Moderate | Progressive disease, mild hypogammaglobulinemia |
| High | History of severe infections, receiving immunosuppressive therapy, profound IgG deficiency |
Routine screening includes:
- Immunoglobulin levels (IgG, IgA, IgM)
- Vaccination history
- Prior infection documentation
- Neutrophil and lymphocyte counts
Immunization Strategies in CLL Patients
Vaccination plays a critical role in bacterial infection prevention, though response rates may be suboptimal in immunocompromised individuals.
Recommended Vaccines
| Vaccine | Indication | Schedule |
|---|---|---|
| Pneumococcal (PCV13 followed by PPSV23) | All CLL patients | PCV13 once, PPSV23 at least 8 weeks later |
| Influenza (Inactivated) | Annual for all patients | Administer pre-treatment or during remission |
| Haemophilus influenzae type B (Hib) | Select high-risk patients | Single dose |
| COVID-19 mRNA Vaccine | Strongly recommended | Follow national guidelines |
Live vaccines are contraindicated in patients with active CLL or those undergoing immunosuppressive therapy.
Antibacterial Prophylaxis in CLL: Guidelines and Regimens
Empirical use of antibiotics may be warranted in high-risk patients, especially those with prior bacterial infections or profound neutropenia.
Indications for Antibacterial Prophylaxis
- Neutrophil count <500/μL (prolonged neutropenia)
- Recurrent lower respiratory tract infections
- Active chemotherapy or BTK inhibitors in patients with low IgG
- Severe hypogammaglobulinemia (IgG <400 mg/dL)
Common Prophylactic Antibiotics
| Antibiotic | Coverage | Typical Use |
|---|---|---|
| Trimethoprim-sulfamethoxazole (TMP-SMX) | Pneumocystis jirovecii, gram-negative rods | CLL on fludarabine or alemtuzumab |
| Levofloxacin | Broad-spectrum gram-positive/negative | Neutropenic prophylaxis |
| Amoxicillin-clavulanate | Community-acquired respiratory pathogens | IgG-deficient patients with chronic infections |
Antibiotic stewardship principles must be applied to minimize resistance and side effects.
Immunoglobulin Replacement Therapy (IGRT)
IGRT is a key intervention for patients with recurrent serious bacterial infections and confirmed hypogammaglobulinemia.
Indications for IGRT
- IgG levels persistently <500 mg/dL
- Two or more serious bacterial infections annually
- Lack of response to vaccination
IGRT Administration
- Intravenous Immunoglobulin (IVIG): 400–600 mg/kg monthly
- Subcutaneous Immunoglobulin (SCIG): Preferred for outpatient self-administration in stable patients
Regular monitoring of IgG trough levels and infection frequency guides dosing and continuation.
Environmental and Lifestyle Modifications
Behavioral interventions reduce exposure to infectious pathogens in immunocompromised CLL patients.
Preventive Measures
- Avoidance of crowded public places during flu season
- Proper food hygiene to prevent gastrointestinal infections
- Pet and zoonotic disease precautions (avoid handling reptiles, clean litter boxes with gloves)
- Hand hygiene and respiratory etiquette education
Travel Considerations
- CLL patients should consult with an infectious disease specialist before traveling
- Region-specific vaccination and antimicrobial prophylaxis may be required
Monitoring and Early Detection of Infections
Prompt recognition and treatment of infections in CLL is essential for favorable outcomes.
Clinical Surveillance Protocol
- Regular temperature monitoring during neutropenic episodes
- Immediate evaluation of respiratory symptoms or fever
- Use of C-reactive protein (CRP) and procalcitonin as infection markers
- Early blood cultures and imaging for suspected deep-seated infections
Patients should receive written action plans for fever and infection management.
Preventing bacterial infections in chronic lymphocytic leukemia demands a multifaceted approach involving risk stratification, immunization, prophylactic antibiotics, and immunoglobulin therapy. Comprehensive infection prevention not only reduces morbidity and mortality but also improves quality of life in patients living with CLL. By implementing personalized prevention strategies and clinical vigilance, we can significantly lower infection-related complications in this vulnerable population.