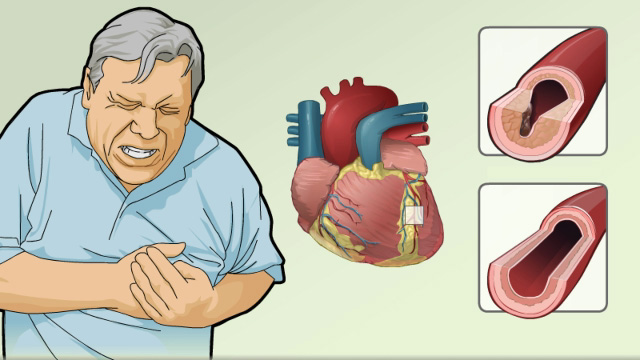
Vasospastic angina, also known as variant angina or Prinzmetal’s angina, is characterized by transient myocardial ischemia caused by reversible coronary artery spasms. Unlike stable angina, vasospastic angina often occurs at rest, particularly during nighttime or early morning hours, and may not be linked to significant atherosclerotic obstruction. Preventing anginal episodes in this context demands a specialized approach focusing on vasodilation, trigger avoidance, and lifestyle optimization.
Understanding Vasospastic Angina and Its Unique Pathophysiology
Vasospastic angina results from episodic constriction of coronary arteries due to hyper-reactivity of vascular smooth muscle cells. It is often associated with endothelial dysfunction and increased sensitivity to vasoconstrictors.
Key Features
- Chest pain at rest, frequently occurring in cycles
- Transient ST-segment elevation during episodes
- Minimal or no coronary artery obstruction on angiography
- Prompt relief with nitrates or calcium channel blockers
Early identification is essential to initiate targeted therapy and avoid complications such as arrhythmias, syncope, or myocardial infarction.
Pharmacologic Treatment for Prevention of Anginal Pain in Vasospastic Angina
Effective medical therapy is the cornerstone of preventing anginal attacks in vasospastic angina. The treatment focuses on relieving vasospasm and preventing recurrence.
Calcium Channel Blockers (CCBs): First-Line Therapy
These agents directly inhibit smooth muscle contraction, preventing coronary artery spasm.
- Dihydropyridines (e.g., amlodipine, nifedipine): Potent vasodilators
- Non-dihydropyridines (e.g., diltiazem, verapamil): Also control heart rate
CCBs are highly effective and should be administered in divided doses or extended-release forms to maintain 24-hour protection.
Nitrates: Adjunctive Therapy
- Isosorbide dinitrate and mononitrate: Prevent recurrent vasospasm by promoting vasodilation
- Should be used with nitrate-free intervals to avoid tolerance
Magnesium Supplementation
Magnesium plays a role in vascular tone regulation. Its deficiency may exacerbate vasospasm.
- Oral or intravenous magnesium may benefit select patients, especially those with documented low levels
Avoidance of Vasoconstrictive Triggers
To prevent angina in vasospastic cases, eliminating known triggers is critical.
Common Triggers to Avoid
- Cigarette smoking – major risk factor and trigger
- Cold exposure
- Emotional stress
- Excess alcohol
- Illicit drug use (e.g., cocaine, amphetamines)
- Hyperventilation or extreme exertion
Medication-Induced Spasm
Certain medications can provoke coronary vasospasm and should be avoided:
- Non-selective beta-blockers
- Sumatriptan and ergot alkaloids
- Decongestants (pseudoephedrine)
Avoiding these agents can significantly reduce the frequency of anginal episodes.
Lifestyle Modifications for Long-Term Prevention
Behavioral and lifestyle adjustments play a pivotal role in reducing the occurrence and severity of vasospastic angina.
Smoking Cessation
- The single most effective intervention
- Reduces endothelial dysfunction and smooth muscle reactivity
Stress Management
- Techniques such as cognitive-behavioral therapy, meditation, and yoga help stabilize autonomic function and prevent vasospasm
Dietary Adjustments
- Low-sodium, heart-healthy diet
- Emphasis on magnesium-rich foods: leafy greens, nuts, whole grains
Sleep and Circadian Rhythm
- Attacks often occur during REM sleep or early morning hours
- Good sleep hygiene and adequate melatonin levels may reduce nocturnal events
Diagnostic Evaluation and Risk Stratification
To tailor preventive strategies, a thorough diagnostic approach is essential.
Diagnostic Tests
- Coronary angiography with provocation testing (e.g., acetylcholine or ergonovine) confirms vasospasm
- ECG during anginal episodes shows transient ST elevation
- Holter monitoring detects arrhythmias or silent ischemia
Risk Assessment
Identify patients with:
- Recurrent angina despite therapy
- Coexisting atherosclerosis
- History of ventricular arrhythmias or cardiac arrest
High-risk patients may require intensive monitoring and hospital-based observation.
Invasive Management and Implantable Devices in Refractory Cases
Although rare, some patients experience drug-resistant vasospastic angina requiring advanced interventions.
Coronary Stenting
- Indicated only if fixed stenosis coexists with vasospasm
- Not typically used for pure vasospastic angina
Implantable Cardioverter-Defibrillator (ICD)
- Considered in patients with prior ventricular arrhythmias or sudden cardiac arrest related to vasospasm
Close follow-up and electrophysiological evaluation guide this decision.
Long-Term Monitoring and Patient Education
Preventive management is incomplete without structured monitoring and continuous patient engagement.
Follow-Up Guidelines
- Regular outpatient reviews every 3–6 months
- Symptom diaries to track anginal episodes
- Monitoring adherence to medication and lifestyle plans
Patient Education
Empowering patients with knowledge on symptom recognition and early intervention reduces emergency events.
- Keep sublingual nitrates accessible at all times
- Educate on when to seek emergency care (e.g., prolonged chest pain, fainting)
The prevention of anginal pain associated with vasospastic angina requires a dedicated approach that targets the unique pathophysiological mechanisms of coronary artery spasm. By using calcium channel blockers, nitrates, and supportive lifestyle changes, we can achieve substantial control of symptoms. Avoiding known triggers, ensuring medication adherence, and ongoing patient education are essential to maintaining long-term wellness and preventing life-threatening complications.