Anginal pain, a hallmark symptom of coronary artery disease (CAD), arises due to myocardial ischemia—when oxygen demand exceeds supply in the heart muscle. Preventing angina is central to managing CAD and improving patient quality of life while reducing the risk of myocardial infarction and sudden cardiac death. An integrated approach combining pharmacological therapy, lifestyle interventions, and risk factor modification offers the most effective strategy for preventing anginal episodes and disease progression.
Understanding Anginal Pain and Coronary Artery Disease
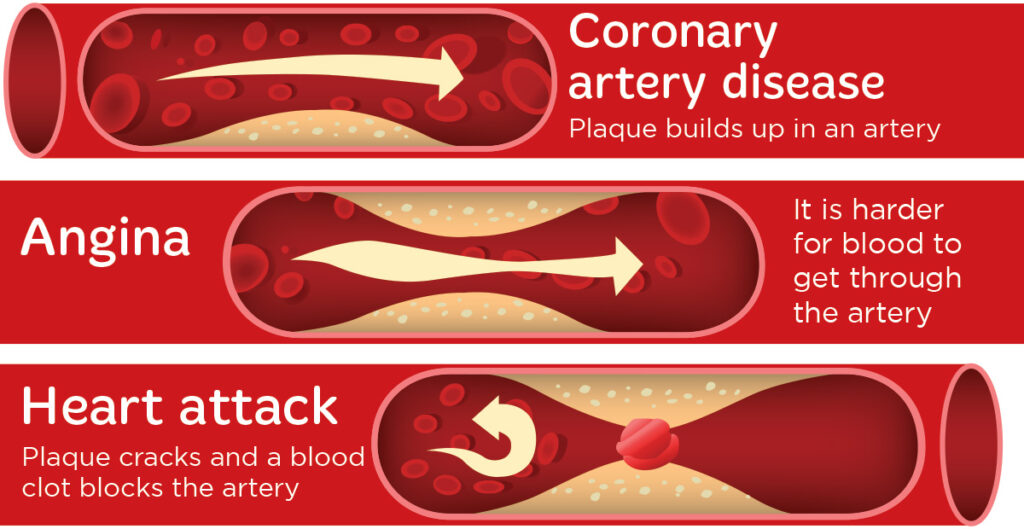
Angina pectoris typically presents as pressure or discomfort in the chest, often triggered by physical exertion or emotional stress. It reflects underlying atherosclerotic narrowing of coronary arteries that impairs oxygen delivery during increased myocardial demand.
There are three primary types of angina:
- Stable angina: Predictable with exertion and relieved by rest or nitrates.
- Unstable angina: Unpredictable, may occur at rest, and represents a medical emergency.
- Variant (Prinzmetal) angina: Caused by coronary artery spasm, typically at rest.
Effective prevention of angina requires controlling the pathophysiological mechanisms of CAD.
Risk Factor Modification: Foundation of Angina Prevention
Aggressive control of modifiable cardiovascular risk factors is essential to reducing angina frequency and progression of coronary artery disease.
Key Modifiable Risk Factors
- Hypertension
- Hyperlipidemia
- Diabetes mellitus
- Smoking
- Obesity
- Sedentary lifestyle
By addressing these elements through evidence-based strategies, we can mitigate ischemic burden and improve vascular function.
Recommended Interventions
- Smoking cessation: Reduces cardiovascular mortality by 36%
- Blood pressure control: Aim for <130/80 mmHg; use ACE inhibitors or ARBs
- Lipid management: Statin therapy to target LDL <70 mg/dL
- Glycemic control: Maintain HbA1c <7% in diabetics
- Weight reduction: 5–10% weight loss lowers inflammatory markers
- Physical activity: At least 150 minutes/week of moderate-intensity aerobic exercise
Pharmacological Therapy to Prevent Anginal Pain
Several drug classes are central to the management and prevention of angina, each targeting distinct physiological pathways to reduce myocardial oxygen demand or improve oxygen supply.
First-Line Agents
- Beta-blockers (e.g., metoprolol, atenolol): Reduce heart rate and myocardial workload
- Calcium channel blockers (e.g., amlodipine, diltiazem): Dilate coronary arteries and lower systemic vascular resistance
- Long-acting nitrates (e.g., isosorbide mononitrate): Prevent vasospasm and decrease preload
Second-Line and Adjunctive Agents
- Ranolazine: Inhibits late sodium current to improve myocardial efficiency
- Ivabradine: Reduces heart rate in patients intolerant to beta-blockers
- Nicorandil: Acts as a nitrate and potassium channel opener
Medications should be titrated based on patient tolerance, symptom burden, and comorbidities.
Antiplatelet and Antithrombotic Therapy
To prevent thrombotic complications that worsen CAD and precipitate unstable angina or myocardial infarction:
- Aspirin (75–100 mg daily): Reduces major adverse cardiovascular events
- Clopidogrel: Alternative or adjunct in aspirin-intolerant patients
- Dual antiplatelet therapy (DAPT): Indicated after PCI with stenting
Long-term adherence is critical for sustained protection.
Coronary Revascularization: PCI and CABG for Refractory Angina
When optimal medical therapy fails to control symptoms, revascularization improves both anginal relief and cardiac outcomes.
Percutaneous Coronary Intervention (PCI)
- Indicated in patients with significant stenosis (>70%) and limiting symptoms
- Stent placement restores blood flow and reduces ischemia
Coronary Artery Bypass Grafting (CABG)
- Recommended for multivessel CAD, left main disease, or diabetics with complex lesions
- Provides long-term symptom relief and mortality benefit
Selection between PCI and CABG depends on anatomical complexity, patient comorbidities, and surgical risk.
Lifestyle and Behavioral Changes for Long-Term Angina Prevention
Non-pharmacological interventions are equally important in preventing anginal episodes and improving cardiovascular prognosis.
Dietary Recommendations
- Mediterranean diet: Rich in olive oil, vegetables, whole grains, and lean protein
- Low sodium intake: <2.3 g/day to control blood pressure
- Limit saturated fats and sugars
Physical Activity
- Aerobic exercise: Walking, swimming, or cycling
- Resistance training: 2–3 sessions per week
- Avoid abrupt intense exertion without warm-up
Stress Management
- Chronic stress exacerbates angina via sympathetic overdrive
- Mindfulness-based stress reduction, yoga, and CBT improve outcomes
Cardiac Rehabilitation: A Structured Preventive Program
Cardiac rehabilitation is a multidisciplinary intervention that significantly reduces angina frequency and cardiovascular events.
Components of Cardiac Rehab
- Supervised exercise training
- Nutritional counseling
- Risk factor education
- Psychosocial support
- Medication adherence monitoring
Patients who complete cardiac rehab experience improved exercise tolerance, quality of life, and reduced hospitalizations.
Monitoring and Follow-Up for Ongoing Angina Prevention
Continual evaluation ensures that therapeutic goals are met and adjusted based on patient progress.
Key Monitoring Parameters
- Symptom diary: Frequency and severity of angina episodes
- Blood pressure and lipid profile
- Medication adherence checks
- Annual stress testing for high-risk patients
Proactive follow-up improves long-term outcomes and prevents silent ischemia.
Preventing anginal pain in patients with coronary artery disease requires a multifaceted, evidence-based approach. Through risk factor modification, individualized pharmacotherapy, lifestyle changes, and interventional strategies when necessary, we can significantly reduce the burden of angina, enhance functional capacity, and prolong life. The integration of medical care with patient education and behavioral transformation is paramount in achieving optimal cardiovascular health.

