Cachexia due to HIV, often referred to as HIV-associated wasting syndrome, is a severe condition marked by unintentional weight loss, muscle atrophy, and systemic inflammation. It remains a significant health challenge for individuals living with HIV, despite advancements in antiretroviral therapy (ART). This article delves into the causes, symptoms, and management strategies for this debilitating condition.
What Is Cachexia?
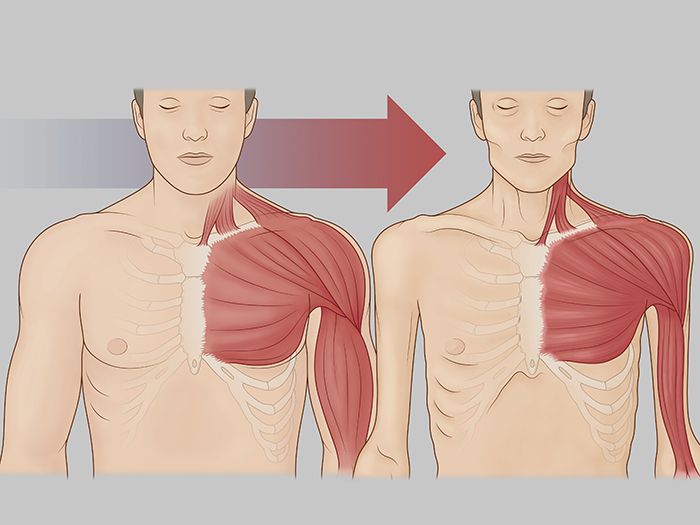
Cachexia is a complex metabolic syndrome characterized by severe weight loss, primarily from muscle rather than fat. Unlike simple starvation, cachexia involves systemic inflammation and metabolic abnormalities, making it resistant to conventional nutritional support. In the context of HIV, cachexia can drastically impair quality of life and increase mortality risk.
Causes of Cachexia in HIV
1. Chronic Inflammation
HIV infection triggers persistent immune activation, leading to the release of pro-inflammatory cytokines like tumor necrosis factor-α (TNF-α), interleukin-1 (IL-1), and interleukin-6 (IL-6). These cytokines play a critical role in muscle catabolism and appetite suppression.
2. Hormonal Dysregulation
Hormonal imbalances, including decreased testosterone levels and altered cortisol production, can exacerbate muscle wasting in individuals with HIV.
3. Malabsorption and Nutritional Deficiencies
HIV-related gastrointestinal complications can impair nutrient absorption, contributing to weight loss and muscle atrophy.
4. Opportunistic Infections
Infections such as tuberculosis and cytomegalovirus can worsen the metabolic disruptions associated with cachexia.
5. Antiretroviral Therapy (ART) Side Effects
While ART has revolutionized HIV care, certain medications may contribute to mitochondrial dysfunction and metabolic changes, indirectly promoting cachexia.
Recognizing the Symptoms
- Unintentional Weight Loss: Defined as a loss of more than 10% of body weight over 6 months.
- Muscle Weakness: Progressive loss of skeletal muscle strength and mass.
- Appetite Changes: Anorexia or reduced food intake due to nausea or oral complications.
- Fatigue: Persistent tiredness and lack of energy.
- Systemic Symptoms: Fever, night sweats, and chronic diarrhea.
Diagnosis of Cachexia in HIV
1. Clinical Assessment
A thorough medical history and physical examination are crucial. Key factors include weight history, dietary intake, and the presence of infections or ART side effects.
2. Laboratory Tests
- Cytokine Levels: Elevated TNF-α and IL-6 are indicative of inflammation.
- Nutritional Markers: Low albumin and prealbumin levels suggest malnutrition.
- Hormonal Analysis: Testosterone and cortisol levels can provide insights into hormonal imbalances.
3. Imaging Studies
Dual-energy X-ray absorptiometry (DEXA) scans can help quantify muscle and fat loss.
Management Strategies
1. Optimized Antiretroviral Therapy (ART)
Effective ART reduces viral load, curbing chronic inflammation and its contribution to cachexia.
2. Nutritional Interventions
- High-Protein Diets: Promote muscle synthesis and repair.
- Micronutrient Supplementation: Address deficiencies in vitamins and minerals.
- Appetite Stimulants: Medications like megestrol acetate can enhance food intake.
3. Physical Rehabilitation
Resistance training and physical activity can counteract muscle wasting and improve overall function.
4. Pharmacological Approaches
- Anti-inflammatory Agents: Target cytokine activity to reduce systemic inflammation.
- Anabolic Steroids: Testosterone supplementation can support muscle growth.
- Cannabinoids: May improve appetite and reduce nausea.
5. Addressing Underlying Conditions
Managing opportunistic infections and gastrointestinal disorders is crucial to improving outcomes.
Prevention
- Early initiation of ART to prevent chronic inflammation and disease progression.
- Regular nutritional assessments and dietary counseling.
- Routine monitoring for opportunistic infections and associated conditions.