Cesarean section (C-section) is a common surgical procedure performed when a vaginal delivery poses risks to the mother or baby. While life-saving, it involves significant postoperative pain due to the incision in the abdominal wall and uterus. Understanding the causes of postoperative pain and implementing effective management strategies is crucial for improving recovery outcomes. This article delves into the factors contributing to postoperative pain after a C-section, provides insight into pain management techniques, and discusses strategies to enhance recovery for new mothers.
Understanding Postoperative Pain After Cesarean Section
Postoperative pain following a cesarean section can range from mild discomfort to intense, localized pain. The pain primarily stems from the surgical incision site, but other factors can contribute to discomfort and recovery time. These factors include surgical trauma, uterine involution, and hormonal changes after childbirth.
Causes of Postoperative Pain
- Surgical Incision
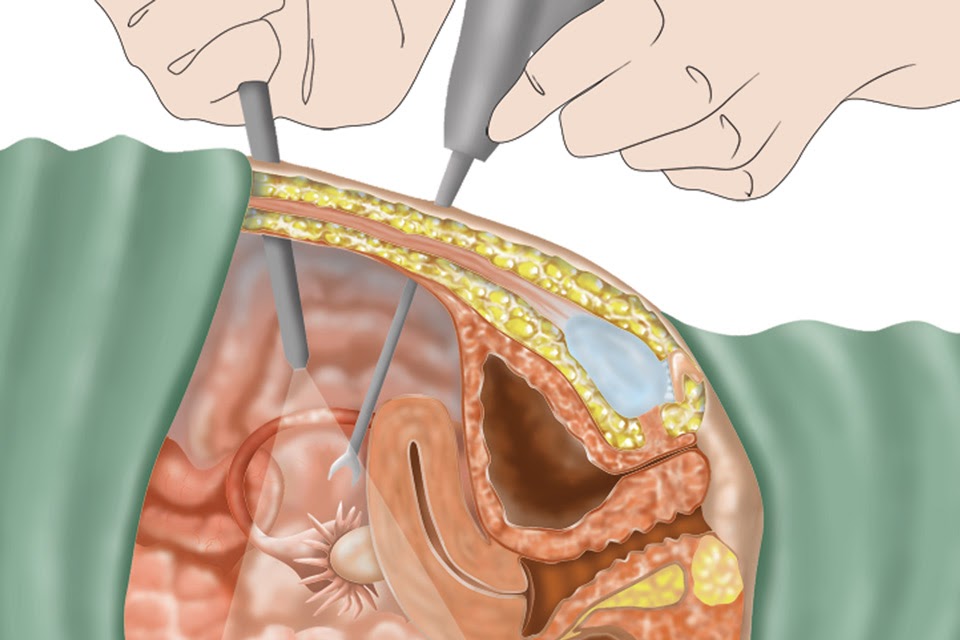
The primary source of pain after a C-section is the incision itself, typically made horizontally across the lower abdomen. This incision cuts through layers of skin, muscle, and fascia, all of which require time to heal. The body’s natural inflammatory response to the incision causes localized pain. - Uterine Involution
After the delivery, the uterus begins to contract and shrink back to its pre-pregnancy size, a process known as uterine involution. This can cause cramping and discomfort, particularly in the first few days after surgery. - Gas and Bloating
Many women experience bloating and discomfort from trapped gas following surgery, especially if the C-section was performed under general anesthesia. The manipulation of the intestines during surgery can lead to temporary digestive disturbances, adding to the pain. - Hormonal Changes
The body undergoes significant hormonal shifts after childbirth. These changes can increase sensitivity to pain and contribute to a feeling of discomfort as the body adjusts.
Types of Postoperative Pain from Cesarean Section
The pain after a C-section may vary in nature and intensity, with different types of pain affecting the recovery experience.
Incisional Pain
Incisional pain is the most common type of postoperative pain. It manifests as a sharp or throbbing sensation at the site of the surgical incision. The pain typically worsens with movement, such as getting in or out of bed, coughing, or laughing. The severity of incisional pain can depend on the surgical technique, the patient’s healing process, and the presence of complications such as infection.
Uterine Cramping
Uterine cramping is common during the early stages of recovery, especially as the uterus contracts to return to its pre-pregnancy size. These cramps are similar to menstrual cramps and can be mild to moderate in intensity. They are often more pronounced when breastfeeding, as breastfeeding stimulates uterine contractions.
Gas and Bloating
Many new mothers experience bloating and discomfort from gas after a C-section. This can cause cramp-like pain in the abdomen, along with feelings of fullness and pressure. The discomfort from bloating usually improves within a few days as the body adjusts to post-surgical recovery.
Pain Management Strategies for Cesarean Section Recovery
Effective pain management is key to a smoother recovery and improved quality of life after a C-section. The goal is to balance adequate pain control while minimizing side effects and promoting healing. Below are the main approaches to managing postoperative pain after cesarean delivery.
Pharmacologic Pain Management
1. Opioids
Opioid medications are typically prescribed for the first few days after surgery for moderate to severe pain. These are often given through an intravenous (IV) line or orally. While effective, opioids have potential side effects, including drowsiness, nausea, and the risk of addiction. As pain decreases, these medications are gradually tapered.
2. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs such as ibuprofen or naproxen are frequently used in combination with opioids to provide additional pain relief. They work by reducing inflammation around the incision site and alleviating mild to moderate pain. NSAIDs can be administered orally or through an IV.
3. Acetaminophen
Acetaminophen is often used for mild pain relief and is considered a safer alternative for those who need to avoid NSAIDs or opioids. It can be taken in combination with other pain relievers for enhanced efficacy.
4. Local Anesthetics
In some cases, a local anesthetic may be applied directly to the incision site. This can offer immediate, short-term relief and reduce the need for stronger oral medications.
Non-Pharmacologic Pain Relief
While medications play a crucial role, non-pharmacologic strategies can significantly improve the comfort and recovery experience after a cesarean section.
1. Cold Compresses
Applying a cold compress to the incision site can help reduce inflammation and provide relief from localized pain. Cold therapy is especially beneficial in the first 48 hours post-surgery.
2. Positioning and Support
Proper positioning, especially when sitting or lying down, can reduce strain on the incision and minimize discomfort. Pillows or cushions can be used to support the abdomen while sleeping or resting.
3. Gentle Movement and Stretching
Gentle walking and light stretching can help prevent stiffness and promote healing. However, patients should avoid lifting heavy objects or performing strenuous activities until advised by their healthcare provider.
4. Breastfeeding Positioning
Breastfeeding can trigger uterine cramping due to the hormone oxytocin. Proper positioning during breastfeeding can help alleviate cramping and prevent unnecessary strain on the incision site.
Preventing Postoperative Pain Complications
To optimize recovery and minimize the risk of complications, several preventive measures should be taken into consideration during the postoperative period.
1. Avoiding Infection
Infection at the surgical site is a major concern after any surgery, including cesarean section. Proper wound care, maintaining cleanliness, and following the healthcare provider’s instructions for bathing and dressing changes are essential to prevent infection.
2. Managing Constipation
Pain medications, especially opioids, can lead to constipation, which exacerbates abdominal discomfort. To prevent constipation, it is important to stay hydrated, consume fiber-rich foods, and follow a healthcare provider’s advice on laxatives or stool softeners.
3. Monitoring for Abnormal Symptoms
Any unusual symptoms, such as increased redness, warmth, swelling, or discharge from the incision site, should be immediately reported to a healthcare provider. These may be signs of infection or complications that require prompt treatment.
Postoperative pain following a cesarean section is a common challenge, but with appropriate pain management, recovery can be smoother and more comfortable. A combination of pharmacologic and non-pharmacologic strategies, coupled with proper wound care and preventive measures, ensures optimal healing. New mothers should work closely with their healthcare team to develop a personalized pain management plan that supports both their physical and emotional well-being as they transition into motherhood. With the right care, the journey toward full recovery can be a positive experience.

