Postmenopausal urethral atrophy is a component of the broader genitourinary syndrome of menopause (GSM), characterized by estrogen deficiency-induced atrophic changes in the urethra, bladder, and surrounding vaginal tissues. This condition affects millions of women globally, impairing urinary function and reducing quality of life. Though underreported and often misdiagnosed, timely recognition and treatment yield significant improvements in symptom control and urogenital health.
Estrogen Deficiency and Urethral Atrophy: The Pathophysiological Basis
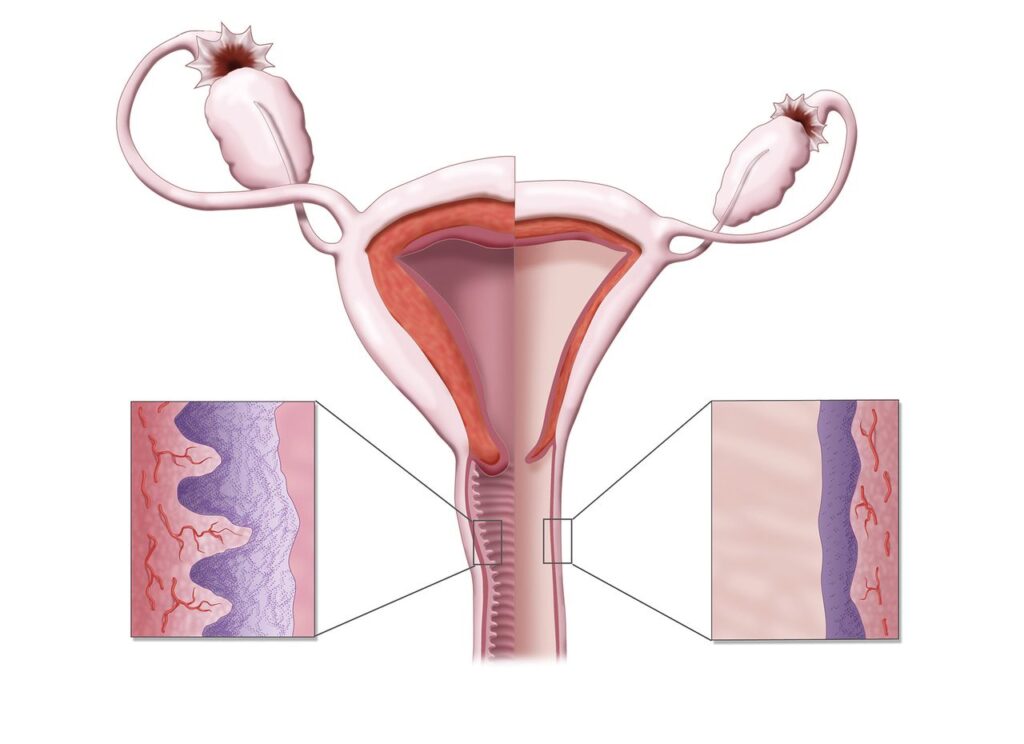
With the cessation of ovarian estrogen production during menopause, urogenital tissues—particularly the urethral epithelium and periurethral structures—undergo atrophic changes. Estrogen plays a critical role in maintaining:
- Urethral mucosal thickness
- Vascularization and elasticity
- Collagen and smooth muscle integrity
- Resistance to infection and irritation
The loss of estrogen leads to thinning of the urethral epithelium, decreased vascularity, and increased susceptibility to trauma and inflammation.
Clinical Presentation: Recognizing the Symptoms
Postmenopausal urethral atrophy may manifest subtly or with distressing urinary and genital complaints. Common symptoms include:
- Dysuria (burning sensation during urination)
- Urinary frequency and urgency
- Post-void dribbling
- Recurrent urinary tract infections (UTIs)
- Urethral discomfort or irritation
- Urinary incontinence (stress or urge-related)
- Dyspareunia (pain during sexual activity) due to associated vaginal atrophy
These symptoms may overlap with other urological or gynecological conditions, necessitating careful evaluation.
Diagnostic Approach: Evaluation of Urethral Atrophy
A thorough diagnostic strategy combines clinical history, physical examination, and investigative tools.
1. Clinical Examination
- Urethral inspection: Reveals pallor, mucosal thinning, and fragility
- Vaginal examination: Often shows coexistent atrophic vaginitis
- Palpation: May elicit tenderness or identify urethral caruncle or prolapse
2. Urinalysis and Culture
To rule out active infection or hematuria
3. Urodynamic Studies
In selected cases with urinary incontinence or voiding dysfunction
4. Cystourethroscopy
Used when hematuria or anatomic abnormality is suspected
Management Strategies: Evidence-Based Treatment Modalities
Treatment of postmenopausal urethral atrophy focuses on restoring local estrogen levels, alleviating symptoms, and preventing recurrence.
Topical Estrogen Therapy: First-Line Intervention
Localized estrogen therapy effectively reverses urethral atrophy without systemic exposure. Options include:
- Estradiol vaginal cream (0.01%): Applied daily for 2 weeks, then 1–3 times weekly
- Vaginal estradiol tablets (10 mcg)
- Estradiol-releasing vaginal ring: Maintains continuous estrogen delivery for 3 months
Benefits:
- Improves urethral epithelial integrity
- Enhances urethral closure pressure
- Reduces urinary symptoms and infection recurrence
Systemic Hormone Replacement Therapy (HRT)
Reserved for women with concurrent menopausal symptoms (e.g., vasomotor instability). Requires risk-benefit assessment due to cardiovascular and oncologic concerns.
Non-Hormonal Therapies
For women who decline or cannot use estrogen:
- Vaginal moisturizers: Provide symptomatic relief
- Vaginal lubricants: Assist with sexual comfort
- Pelvic floor exercises: Strengthen urethral support
- Laser therapy (CO₂ or erbium): Promotes mucosal regeneration via photothermal effects
Preventing Recurrent Infections and Urinary Symptoms
Addressing urethral atrophy reduces recurrent UTIs and urinary dysfunction. Preventive strategies include:
- Maintaining regular estrogen therapy
- Adequate hydration
- Avoiding irritants (e.g., perfumed products, harsh soaps)
- Prophylactic low-dose antibiotics in recurrent UTI cases
- Cranberry supplements or D-mannose (as adjuncts)
Quality of Life Impact and Patient Counseling
Left untreated, urethral atrophy significantly impairs daily functioning and emotional wellbeing. Patient education is vital in encouraging open dialogue and adherence to long-term therapy. Topics to discuss include:
- Treatment safety and effectiveness
- Long-term maintenance strategies
- Monitoring for symptom recurrence
- Addressing sexual health concerns
Empowering patients with information fosters confidence in managing this often overlooked but impactful condition.
Postmenopausal urethral atrophy is a prevalent yet frequently underdiagnosed component of genitourinary syndrome of menopause. Prompt recognition, individualized therapy—primarily with topical estrogen—and long-term symptom monitoring can dramatically improve patient outcomes. An integrative approach involving education, lifestyle modification, and regular follow-up ensures sustained urethral and urogenital health.