Postencephalitic parkinsonism (PEP) is a rare, neurodegenerative condition resulting from viral encephalitis, most notably encephalitis lethargica. It is characterized by Parkinson-like motor symptoms including bradykinesia, rigidity, tremor, and postural instability. First observed following the global encephalitis lethargica epidemic from 1917 to 1928, this condition primarily affects the extrapyramidal system, with lasting neurological sequelae.
Historical Context: Encephalitis Lethargica and Its Aftermath
The largest known outbreak of encephalitis lethargica gave rise to thousands of cases of postencephalitic parkinsonism. Affected individuals initially presented with flu-like symptoms, progressing to neurological decline. Months to years after the acute infection, survivors frequently developed parkinsonian syndromes, implicating viral damage to basal ganglia structures.
Pathophysiology: Brain Changes in PEP
The pathogenesis of postencephalitic parkinsonism involves neuronal degeneration in the substantia nigra pars compacta, a midbrain region critical for dopamine production. This degeneration leads to the hallmark features of parkinsonism due to dopamine deficiency in the striatum.
Key Pathological Findings:
- Loss of pigmented neurons in the substantia nigra
- Gliosis in the midbrain and basal ganglia
- Inflammatory changes suggestive of prior viral insult
- Absence of Lewy bodies (unlike idiopathic Parkinson’s disease)
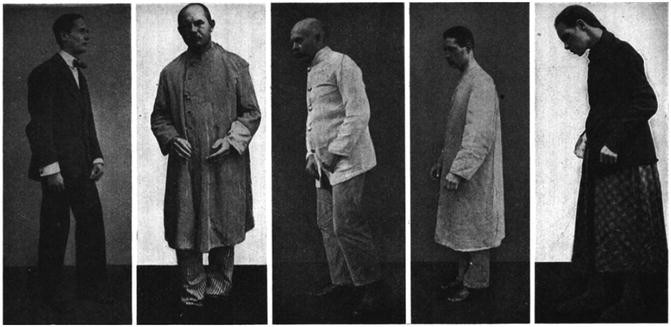
Clinical Presentation of Postencephalitic Parkinsonism
Motor Symptoms:
- Bradykinesia: Slowness of voluntary movement
- Rigidity: Increased muscle tone, often lead-pipe or cogwheel in nature
- Tremor: Typically resting tremor affecting limbs
- Postural Instability: Impaired balance and increased fall risk
Non-Motor Symptoms:
- Oculogyric crises: Involuntary upward deviation of the eyes
- Speech impairment: Monotone, reduced volume, or dysarthria
- Cognitive changes: Memory disturbances, apathy, or mood disorders
- Sleep disturbances and autonomic dysfunction
Diagnostic Approach
Accurate diagnosis of postencephalitic parkinsonism hinges on thorough history and clinical evaluation. Key features include a history of encephalitic illness followed by a latent period and subsequent onset of parkinsonism.
Diagnostic Tools:
- MRI Brain: May reveal atrophy in basal ganglia and midbrain
- DaTSCAN: Shows reduced dopamine transporter activity
- CSF Analysis: Typically nonspecific but helps exclude other infections
- Neuropsychological Testing: Identifies cognitive and behavioral impairments
Differential Diagnosis
Postencephalitic parkinsonism must be distinguished from other parkinsonian syndromes:
| Condition | Key Distinctions |
|---|---|
| Idiopathic Parkinson’s Disease | Progressive with Lewy bodies, no viral link |
| Drug-Induced Parkinsonism | Linked to antipsychotics or metoclopramide |
| Vascular Parkinsonism | Associated with cerebrovascular disease |
| Progressive Supranuclear Palsy | Prominent vertical gaze palsy |
Treatment Strategies for PEP
Treatment is largely symptomatic, focusing on managing parkinsonism and improving quality of life.
Pharmacologic Interventions:
- Levodopa/Carbidopa: Modest benefit; responsiveness is variable
- Anticholinergics (e.g., trihexyphenidyl): May alleviate rigidity and tremor
- Dopamine agonists: Sometimes used but limited due to side effects
- Amantadine: Useful for both motor symptoms and fatigue
Non-Pharmacologic Management:
- Physical Therapy: Enhances mobility and reduces rigidity
- Speech Therapy: Addresses dysarthria and communication challenges
- Occupational Therapy: Improves activities of daily living
- Neuropsychiatric Support: Critical for managing depression and cognitive deficits
Prognosis and Long-Term Outlook
The course of postencephalitic parkinsonism varies by individual, with some experiencing progressive decline while others stabilize with symptomatic management. Unlike idiopathic Parkinson’s disease, PEP is not typically associated with Lewy body pathology, which may influence long-term trajectory and treatment responsiveness.
Prevention and Research Directions
Since postencephalitic parkinsonism stems from viral encephalitis, prevention depends on effective public health measures to control infections, including vaccination and surveillance. Research is ongoing to better understand viral mechanisms of neurodegeneration and to explore disease-modifying therapies.
Postencephalitic parkinsonism remains a rare but historically significant condition rooted in viral CNS insult. Understanding its pathophysiology, recognizing clinical signs, and applying targeted therapies are essential for improving patient outcomes. Vigilant monitoring, comprehensive rehabilitation, and advances in neurotherapeutics hold promise for better management of this complex syndrome.