Postabortal hemorrhage refers to excessive bleeding following a spontaneous or induced abortion. As one of the most serious complications of abortion, it demands immediate recognition and prompt intervention. Defined as blood loss exceeding 500 mL or any amount resulting in hemodynamic instability, postabortal hemorrhage can arise from various etiologies including uterine atony, retained products of conception, or trauma to reproductive organs.
Causes and Risk Factors for Postabortal Hemorrhage
Uterine Atony
The most common cause of postabortal hemorrhage is uterine atony, wherein the uterus fails to contract effectively after abortion, leading to ongoing bleeding from the placental site.
Retained Products of Conception (RPOC)
Incomplete evacuation of fetal or placental tissue hinders effective uterine contraction, perpetuating hemorrhage.
Cervical or Uterine Trauma
Instrumentation during surgical abortion may cause cervical lacerations or uterine perforation, both of which are significant sources of bleeding.
Coagulopathies
Underlying bleeding disorders, whether known or undiagnosed, can exacerbate postabortion bleeding.
Infection
Endometritis or septic abortion can compromise uterine tone and coagulation, intensifying blood loss.
Risk Enhancers:
- Advanced gestational age at abortion
- History of multiple abortions
- Inadequate cervical preparation
- Use of sharp curettage
- Previous cesarean section or uterine surgery
Classification of Hemorrhage Severity
| Severity | Blood Loss Estimate | Clinical Signs |
|---|---|---|
| Mild | <500 mL | Minimal hemodynamic impact |
| Moderate | 500–1000 mL | Tachycardia, mild hypotension |
| Severe | >1000 mL | Hypotension, pallor, altered mentation |
Clinical Presentation and Assessment
Patients experiencing postabortal hemorrhage typically present with:
- Persistent or profuse vaginal bleeding
- Lower abdominal pain
- Dizziness or syncope
- Hypotension and tachycardia
- Uterine tenderness (in cases of retained tissue or infection)
Evaluation Includes:
- Vital signs and hemodynamic assessment
- Bimanual examination: Assess uterine size and tone
- Speculum examination: Identify cervical lacerations or active bleeding source
- Ultrasound imaging: Evaluate for RPOC, uterine perforation, or hematometra
- Laboratory tests: CBC, coagulation profile, blood type, and crossmatch
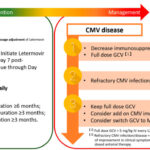
Management Protocols for Postabortal Hemorrhage
Initial Stabilization
- Establish IV access with large-bore cannulas
- Begin fluid resuscitation with crystalloids
- Administer oxygen as needed
- Crossmatch blood for possible transfusion
Definitive Management Based on Cause
Uterine Atony
- Uterine massage
- Uterotonic agents:
- Oxytocin (IV)
- Methylergometrine (IM)
- Misoprostol (rectal or sublingual)
- Carboprost (IM, contraindicated in asthma)
Retained Products of Conception
- Ultrasound confirmation
- Suction curettage or manual vacuum aspiration
- Antibiotic prophylaxis if infection is suspected
Cervical or Vaginal Lacerations
- Direct visualization and suturing of tears under anesthesia
Uterine Perforation
- Suspected when uterus is soft and bleeding persists with no RPOC
- May require laparoscopic or open surgical repair
Coagulopathy
- Administer platelets, fresh frozen plasma, or specific factors based on lab findings
Preventive Strategies in Abortion Care
Effective prevention of postabortal hemorrhage involves meticulous attention to technique and patient selection.
Cervical Preparation
Use of misoprostol or osmotic dilators before surgical abortion reduces trauma and facilitates easier evacuation.
Skilled Providers
Procedures conducted by trained clinicians drastically reduce complication rates.
Ultrasound Guidance
Ensures complete evacuation, minimizes risk of perforation or RPOC.
Prophylactic Uterotonics
Routine use after abortion, especially in high-risk cases, decreases uterine atony incidence.
Post-Procedure Monitoring
Observe patients for 1–2 hours post-abortion to detect early signs of hemorrhage.
When to Escalate Care
Escalation is warranted if:
- Bleeding exceeds 1000 mL or patient is unstable
- No response to uterotonics or evacuation
- Suspicion of uterine rupture or unrecognized perforation
- Evidence of DIC (Disseminated Intravascular Coagulation)
Transfer to a higher-level facility may be necessary for surgical intervention, interventional radiology (uterine artery embolization), or intensive care support.
Postabortal hemorrhage is a critical complication that requires immediate recognition and targeted intervention to ensure patient safety. With structured protocols, skilled care, and preventive measures, we can significantly reduce morbidity and mortality associated with postabortion bleeding. Empowering healthcare systems with training and resources is vital to delivering safe abortion care globally.