Post-operative vaginal cuff infections represent a serious complication following gynecologic surgeries, particularly total hysterectomy. Among the microbial culprits, Peptostreptococcus—an anaerobic Gram-positive coccus—frequently colonizes the female genital tract and may cause deep pelvic infections when introduced to surgical sites.
Understanding the etiology, clinical presentation, diagnostic approach, and management of Peptostreptococcus infections following vaginal cuff procedures is critical in optimizing patient outcomes and minimizing morbidity.
Etiology: Peptostreptococcus as a Post-Surgical Pathogen
Peptostreptococcus species are part of the normal flora of the gastrointestinal, oral, and vaginal tracts. These anaerobes can become pathogenic in immunocompromised states or following surgical trauma, particularly when mucosal barriers are breached.
During procedures like total abdominal or vaginal hysterectomy, exposure of sterile surgical fields to endogenous anaerobes can initiate infection. Infections at the vaginal cuff are especially vulnerable due to the moist, low-oxygen environment conducive to anaerobic proliferation.
Risk Factors for Vaginal Cuff Peptostreptococcus Infection
Several predisposing factors increase susceptibility to post-hysterectomy infections by Peptostreptococcus:
- Impaired aseptic technique during closure of the vaginal cuff
- Prolonged operative time
- Excessive intraoperative blood loss
- Use of vaginal instrumentation
- Poorly controlled diabetes mellitus
- Obesity or smoking history
- Pre-existing bacterial vaginosis or pelvic inflammatory disease
Postmenopausal women with thinner vaginal epithelium and reduced vascularity may also face higher risk due to slower wound healing.
Clinical Presentation and Symptoms
The hallmark of a vaginal cuff infection is delayed post-operative pelvic pain accompanied by systemic or localized signs of infection. Specific manifestations of Peptostreptococcus infection may include:
- Foul-smelling vaginal discharge
- Persistent low-grade fever
- Deep pelvic pain or dyspareunia
- Vaginal cuff dehiscence in severe cases
- Pelvic abscess or parametrial phlegmon formation
These symptoms often manifest 5–14 days post-surgery, though they can occasionally be delayed.
Diagnostic Approach
Timely diagnosis hinges on a combination of clinical evaluation, imaging, and microbiological analysis.
1. Physical Examination
- Bimanual exam reveals cervical motion tenderness or fullness in the vaginal fornix.
- Visualization may show inflammation, discharge, or cuff separation.
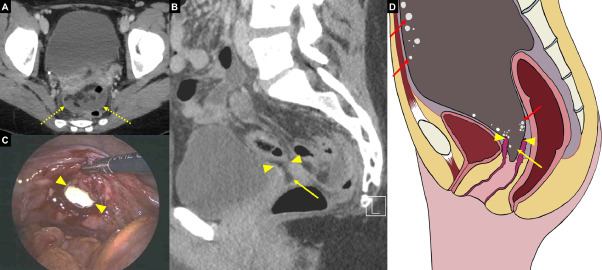
2. Imaging Studies
- Transvaginal ultrasound may detect fluid collection or abscess.
- CT pelvis with contrast is superior in identifying deep space infections and abscesses.
3. Microbiologic Confirmation
- Vaginal or cuff swabs should be cultured under anaerobic conditions.
- Peptostreptococcus is slow-growing and often requires extended incubation (up to 5–7 days).
- Blood cultures may be positive in advanced or systemic cases.
Optimal Treatment Strategies
1. Antibiotic Therapy
Early empiric therapy is essential, later refined based on culture sensitivity. Treatment should target anaerobes:
- First-line regimen:
- IV ampicillin-sulbactam or
- IV clindamycin plus gentamicin
- Oral step-down: After clinical improvement, transition to amoxicillin-clavulanate or metronidazole plus doxycycline for 10–14 days.
Resistance patterns should be monitored, as Peptostreptococcus may display beta-lactamase production.
2. Surgical Intervention
- Necessary in cases of abscess, necrotizing infection, or cuff dehiscence.
- Procedures may include:
- Abscess drainage
- Re-suturing of the vaginal cuff
- Debridement of necrotic tissue
3. Supportive Care
- Adequate fluid hydration
- Pain control with non-opioid analgesics
- Close monitoring for signs of sepsis or systemic spread
Preventive Measures and Best Practices
Preventing vaginal cuff infections, especially from anaerobes like Peptostreptococcus, requires vigilant perioperative protocols:
- Preoperative vaginal cleansing with povidone-iodine
- Prophylactic antibiotics administered within 60 minutes prior to incision (e.g., cefazolin or cefotetan)
- Minimizing operative time and avoiding unnecessary instrumentations
- Postoperative hygiene education for patients
Use of sutures instead of staples for vaginal cuff closure may reduce infection risk due to better mucosal apposition and healing.
Outcomes and Prognosis
When treated promptly, most patients recover fully with minimal sequelae. However, delayed treatment can result in:
- Chronic pelvic pain
- Formation of adhesions
- Recurrent infections
- Rarely, systemic anaerobic sepsis
Therefore, early recognition, aggressive treatment, and comprehensive post-surgical care are critical to preventing complications.
Peptostreptococcus is an opportunistic pathogen with the potential to cause serious vaginal cuff infections following gynecological surgery. A systematic approach involving early detection, anaerobe-targeted therapy, and surgical management where necessary ensures favorable outcomes. Adherence to perioperative preventive measures is essential in minimizing the incidence of this post-operative complication and preserving patient safety.