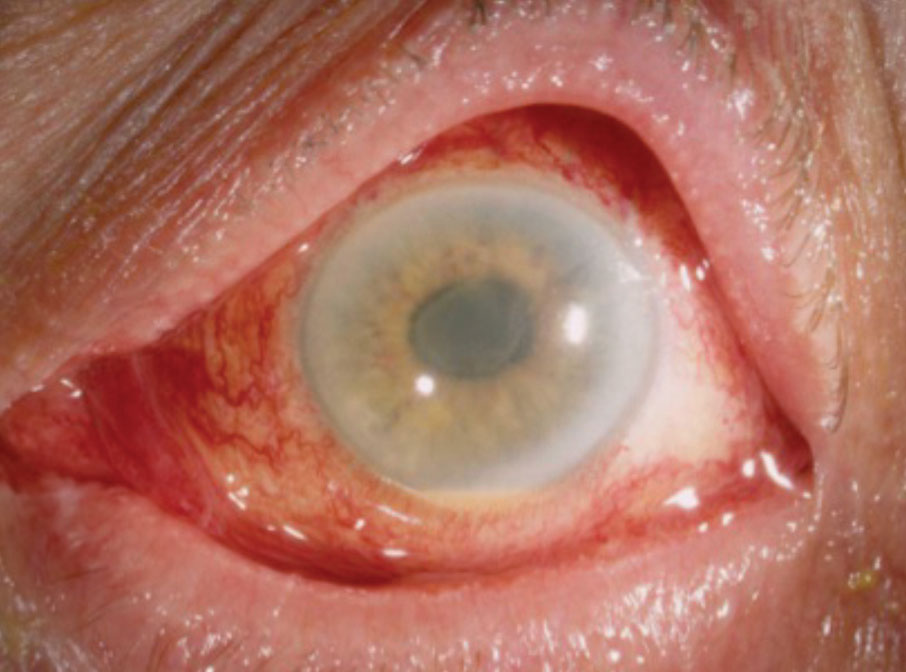
Post-operative ocular inflammation is a common response following various types of intraocular surgery, including cataract extraction, vitrectomy, and glaucoma procedures. While a mild inflammatory reaction is expected, excessive or prolonged inflammation may signify complications such as infection, tissue reaction, or iatrogenic injury. Timely recognition and management are essential to preserving vision and preventing structural damage.
Causes of Post-Operative Ocular Inflammation
Expected vs. Pathological Inflammation
Post-op inflammation ranges from normal immune response to sight-threatening complications. Differentiating between the two is critical.
Common Etiologies:
- Surgical trauma to intraocular tissues
- Retained lens fragments or intraocular foreign bodies
- Toxic anterior segment syndrome (TASS)
- Infectious endophthalmitis
- Prolonged intraoperative time or poor wound closure
- Use of certain intraocular medications or preservatives
Types of Post-Operative Ocular Inflammatory Conditions
1. Anterior Uveitis
- Most common and often mild
- Occurs within 24–72 hours after surgery
- Presents with cells and flare in the anterior chamber
2. Cystoid Macular Edema (CME)
- Fluid accumulation in the macula
- Typically delayed, appearing weeks post-surgery
- May cause blurry or distorted central vision
3. Endophthalmitis
- Rare but severe intraocular infection
- Presents within days to weeks post-op
- Characterized by pain, redness, decreased vision, hypopyon
4. Toxic Anterior Segment Syndrome (TASS)
- Sterile inflammatory reaction
- Rapid onset (<24 hours), painless, with significant AC reaction
- Typically caused by contaminants during surgery
Symptoms and Clinical Presentation
Patients with post-op ocular inflammation may present with a variety of symptoms depending on the severity and type of reaction.
Typical Symptoms:
- Ocular redness
- Pain or discomfort
- Photophobia
- Blurred or decreased vision
- Floaters (in posterior segment involvement)
- Eyelid swelling and discharge (in infectious cases)
Diagnostic Approach to Post-Operative Ocular Inflammation
A systematic approach is necessary for accurate differentiation between infectious and non-infectious causes.
Key Diagnostic Steps:
1. History and Clinical Timeline
- Type of surgery performed
- Time of onset of symptoms post-surgery
- Any intraoperative complications or retained material
2. Slit Lamp Examination
- Assessment of anterior chamber cells and flare
- Identification of hypopyon, keratic precipitates, corneal edema
3. Fundus Evaluation
- Evaluate for CME, vitritis, or retinal involvement
4. Imaging and Ancillary Testing
- OCT (Optical Coherence Tomography) for CME
- B-scan ultrasonography for posterior segment evaluation if media is opaque
- Aqueous/vitreous tap and cultures for suspected endophthalmitis
Treatment Strategies Based on Etiology
1. Mild Inflammatory Reactions
- Topical corticosteroids (e.g., prednisolone acetate)
- Cycloplegic agents to relieve ciliary spasm
2. Cystoid Macular Edema
- Topical NSAIDs (e.g., ketorolac, bromfenac)
- Steroids (topical, periocular, or systemic)
- Anti-VEGF agents in chronic or resistant cases
3. Toxic Anterior Segment Syndrome (TASS)
- Aggressive topical steroids
- IOP monitoring
- No role for antibiotics
4. Infectious Endophthalmitis
- Emergency intravitreal antibiotics
- Vitrectomy in severe cases
- Systemic antibiotics depending on culture results
Prevention of Post-Operative Inflammation
Surgical Techniques and Sterility:
- Meticulous aseptic protocol
- Adequate wound sealing
- Avoidance of toxic contaminants (e.g., non-sterile instruments, preservatives)
Prophylactic Medications:
- Topical antibiotics pre- and post-operatively
- Use of intracameral antibiotics (e.g., cefuroxime)
Patient Factors:
- Control of systemic inflammatory conditions
- Adherence to post-op medication regimen
Prognosis and Long-Term Outcomes
When identified and managed promptly, most forms of post-operative ocular inflammation resolve without permanent vision loss. However, delayed diagnosis, particularly in cases of infectious endophthalmitis, can result in irreversible vision impairment or loss of the eye. Consistent follow-up and patient education are critical for ensuring optimal recovery.
Post-operative ocular inflammation encompasses a spectrum of conditions from benign to vision-threatening. A thorough understanding of its etiologies, clinical features, and management protocols ensures optimal care following intraocular procedures. Through vigilant monitoring and timely intervention, we can mitigate complications and support successful surgical outcomes.