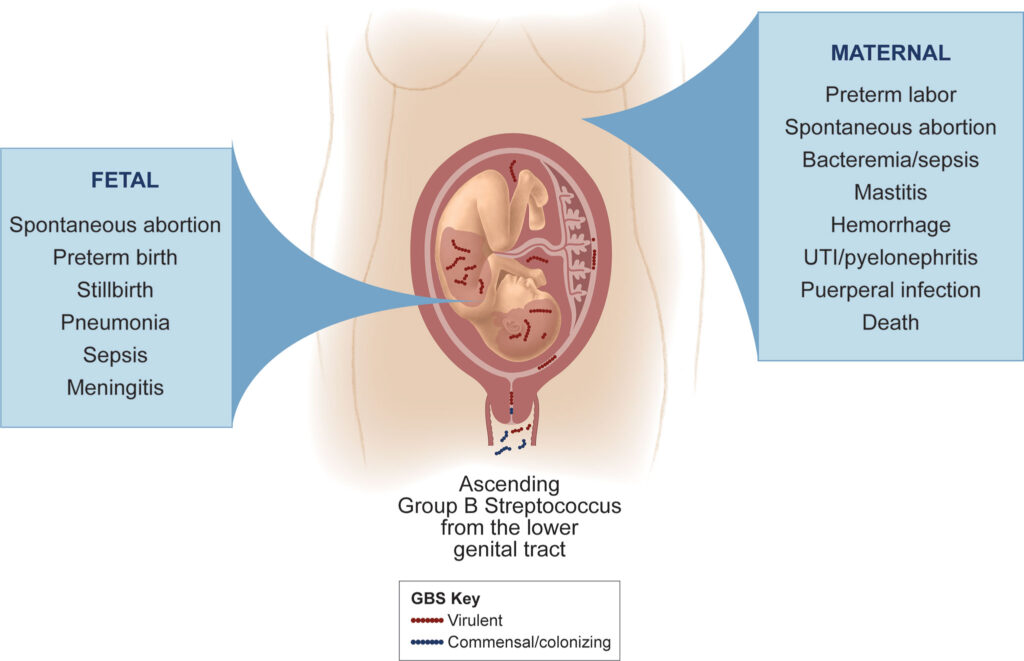
Streptococcus species represent a significant cause of postoperative gynecologic infections, particularly after procedures involving the uterus, fallopian tubes, ovaries, and adjacent pelvic structures. Group A Streptococcus (Streptococcus pyogenes) and Group B Streptococcus (Streptococcus agalactiae) are primary culprits, though other strains such as Streptococcus anginosus group can contribute to deep-seated abscesses and endometritis. Prompt diagnosis and treatment are essential to prevent severe complications including septic shock and infertility.
Pathogenesis: How Streptococcus Causes Infection After Surgery
Colonization to Invasion: Mechanisms of Pathogenicity
Streptococcus species transition from commensals to pathogens when surgical breaches provide access to sterile pelvic environments. Key pathogenic mechanisms include:
- Adhesion to epithelial cells via fibronectin-binding proteins.
- Tissue invasion using streptolysins and hyaluronidase.
- Superantigen production in S. pyogenes triggering systemic inflammation.
- Capsule formation to evade immune clearance.
- Biofilm formation, especially in S. agalactiae, facilitating chronic infection.
These mechanisms lead to rapid proliferation within surgical sites, escalating inflammation and tissue destruction.
Risk Factors Predisposing to Streptococcal Post-Gynecologic Infections
Patients undergoing gynecologic surgery are at increased risk due to a combination of host and procedural factors, including:
- Prolonged labor and premature rupture of membranes
- Cesarean section or hysterectomy
- Multiple vaginal examinations or instrumentation
- Preexisting vaginal Streptococcus colonization
- Immunocompromised status or poorly controlled diabetes
- Non-sterile surgical environments or inadequate prophylaxis
Clinical Presentation and Symptoms of Streptococcus-Related Gynecologic Infections
Typical Onset and Key Indicators
Postoperative Streptococcal infections generally manifest within 48–96 hours post-surgery. Clinicians should remain vigilant for:
- High-grade fever (≥39°C)
- Sudden-onset pelvic or lower abdominal pain
- Purulent vaginal discharge
- Tachycardia, hypotension (in severe cases)
- Marked leukocytosis with left shift
- Signs of toxic shock syndrome (rash, multi-organ involvement)
In rare but critical cases, Group A Streptococcus may trigger Streptococcal Toxic Shock Syndrome (STSS)—a life-threatening condition requiring intensive care.
Diagnostic Evaluation of Streptococcal Postoperative Infections
Laboratory Investigations
- CBC with differential: Leukocytosis with neutrophilia.
- C-reactive protein (CRP) and Procalcitonin: Elevated in systemic involvement.
- Blood cultures: Essential in suspected sepsis.
- High vaginal or endometrial swabs: Culture and sensitivity testing to identify Streptococcus strain.
- Rapid antigen detection tests (RADT): For S. pyogenes in acute settings.
Imaging Modalities
- Pelvic Ultrasound: To detect abscesses or fluid collection.
- CT or MRI with contrast: Identifies deep pelvic or retroperitoneal spread.
- Echocardiography: In cases of bacteremia to rule out endocarditis.
Treatment of Postoperative Streptococcal Gynecologic Infections
Antibiotic Therapy
Immediate initiation of broad-spectrum antibiotics is imperative, followed by targeted therapy based on culture results:
- Empirical Treatment:
- Clindamycin + Penicillin G (especially for Group A Streptococcus)
- Ampicillin + Gentamicin for broader gram-positive and gram-negative coverage
- Vancomycin in cases of suspected resistance or allergy
- Targeted Therapy:
- Group A Streptococcus: High-dose IV Penicillin + Clindamycin
- Group B Streptococcus: Ampicillin or Cefazolin, adjusted for sensitivities
- Duration:
- Typically 10–14 days, extended if abscess or sepsis is present.
Surgical and Supportive Measures
- Drainage of pelvic abscesses: Via imaging-guided aspiration or laparoscopy.
- Debridement of infected surgical sites: Especially for necrotizing fasciitis.
- Hemodynamic stabilization: IV fluids, vasopressors in septic shock.
- Intravenous immunoglobulin (IVIG): Considered in STSS for toxin neutralization.
Prevention of Streptococcal Infections After Gynecologic Surgery
Preoperative Measures
- Routine screening for Group B Streptococcus (GBS) in pregnant or high-risk patients.
- Antibiotic prophylaxis during C-section or open gynecologic surgeries.
- Proper antiseptic preparation of the vaginal and abdominal surgical field.
- Limiting duration and frequency of vaginal examinations during labor.
Intraoperative and Postoperative Care
- Sterile technique adherence
- Shortening surgical duration
- Minimizing foreign body insertion (catheters, sponges)
- Postoperative monitoring for early signs of infection
Complications of Untreated Streptococcal Infections in the Pelvis
If Streptococcal infections are left untreated or inadequately managed, complications can be severe and life-threatening:
- Pelvic or tubo-ovarian abscess
- Peritonitis and sepsis
- Streptococcal toxic shock syndrome
- Infertility due to tubo-peritoneal adhesions
- Necrotizing soft tissue infections requiring extensive surgery
- Death in cases of systemic multi-organ failure
Frequently Asked Questions
What causes postoperative gynecologic infections due to Streptococcus?
They occur when surgical disruption allows Streptococcus species to invade normally sterile pelvic tissues, triggering inflammation and infection.
How serious is a Streptococcus infection after surgery?
It can range from mild endometritis to severe sepsis and toxic shock syndrome, which can be fatal without immediate treatment.
Which antibiotics are effective against Streptococcus species?
Penicillin, clindamycin, and ampicillin are primary treatments. Resistance patterns should guide specific choices.
Can Streptococcal infections be prevented in gynecologic surgery?
Yes, with proper antisepsis, antibiotic prophylaxis, and minimizing invasive procedures during and after surgery.
What are the signs of toxic shock syndrome after surgery?
High fever, rash, hypotension, confusion, and multi-organ dysfunction—prompt ICU care is critical.
Postoperative gynecologic infections due to Streptococcus demand rapid identification and aggressive therapy to avoid serious morbidity or mortality. Understanding the pathogenesis, recognizing risk factors, and implementing precise antibiotic and surgical interventions are paramount. Clinicians must remain vigilant in both prevention and early management to ensure optimal outcomes in surgical gynecology.