Bancroft’s filariasis, also referred to as lymphatic filariasis, is a parasitic disease caused by Wuchereria bancrofti. This condition is transmitted to humans through mosquito bites and primarily affects the lymphatic system, leading to chronic disability and disfigurement. It is prevalent in tropical and subtropical regions, particularly in areas with inadequate sanitation and high mosquito density. This article delves into the causes, symptoms, diagnostic methods, treatment, and prevention of Bancroft’s filariasis.
Causes and Transmission
Bancroft’s filariasis is caused by the filarial nematode Wuchereria bancrofti. The parasite completes its life cycle within two hosts: mosquitoes (vector) and humans (definitive host).
Life Cycle of Wuchereria bancrofti
- Mosquito Infection: Female mosquitoes (primarily Culex, Anopheles, and Aedes species) ingest microfilariae while feeding on infected human blood.
- Larval Development: Microfilariae develop into infective larvae (L3 stage) within the mosquito.
- Human Infection: During subsequent bites, infective larvae enter the human bloodstream.
- Lymphatic Colonization: Larvae migrate to the lymphatic vessels, maturing into adult worms. These worms produce microfilariae, perpetuating the cycle.
Symptoms and Clinical Manifestations
The clinical presentation of Bancroft’s filariasis varies based on the stage of infection:
Acute Phase
- Filarial Fever: Sudden onset of fever and chills.
- Lymphangitis: Painful inflammation of lymphatic vessels.
- Lymphadenitis: Swelling and tenderness of lymph nodes.
Chronic Phase
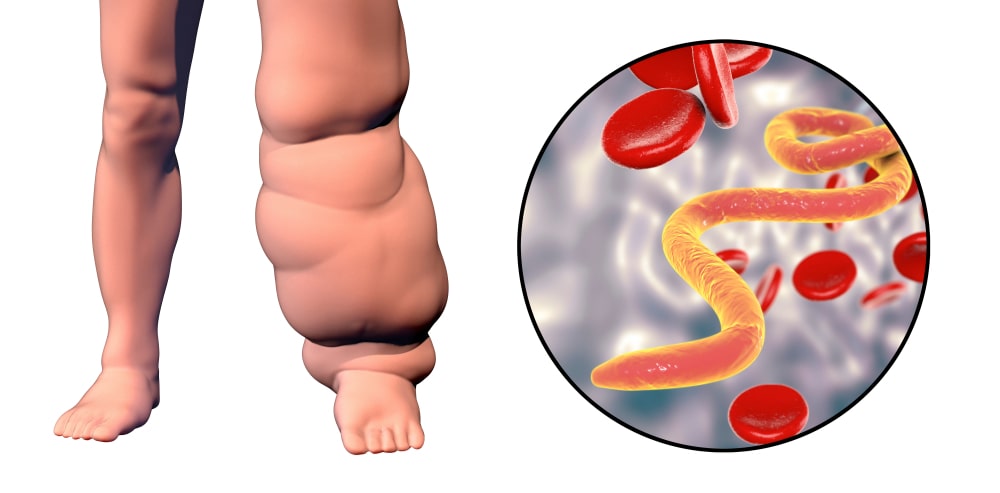
- Lymphedema: Persistent swelling, typically in the limbs, due to impaired lymphatic drainage.
- Hydrocele: Accumulation of fluid in the scrotum, commonly seen in males.
- Elephantiasis: Severe thickening and hardening of the skin, leading to disability and social stigma.
Diagnosis
Accurate diagnosis is essential for effective management. The following methods are commonly used:
Microscopic Examination
- Blood smear analysis detects microfilariae in peripheral blood samples.
- Specimens are best collected at night (nocturnal periodicity).
Immunological Tests
- Antigen detection tests, such as ELISA, identify specific filarial antigens.
- Antibody tests assess immune response to the parasite.
Imaging Techniques
- Ultrasound can detect adult worms in lymphatic vessels (“filarial dance sign”).
- Lymphoscintigraphy evaluates lymphatic dysfunction.
Treatment Options
Management of Bancroft’s filariasis involves eliminating the parasite and addressing complications:
Pharmacological Treatment
- Diethylcarbamazine (DEC): Kills microfilariae and adult worms.
- Ivermectin: Effective against microfilariae, often combined with DEC or albendazole.
- Albendazole: Targets adult worms and is used in combination therapy.
Supportive Care
- Hygiene Practices: Daily cleaning and moisturizing of affected areas prevent secondary infections.
- Compression Therapy: Reduces swelling in lymphedema.
- Surgical Intervention: Corrective procedures for hydrocele or advanced lymphedema.
Prevention and Control
Preventing Bancroft’s filariasis requires integrated vector control and community health initiatives:
Vector Control
- Use of insecticide-treated bed nets (ITNs).
- Indoor residual spraying (IRS) with effective insecticides.
- Elimination of mosquito breeding sites.
Mass Drug Administration (MDA)
- WHO recommends periodic administration of antifilarial drugs to at-risk populations.
Health Education
- Raising awareness about the disease and its prevention.
- Encouraging early treatment and vector control practices.