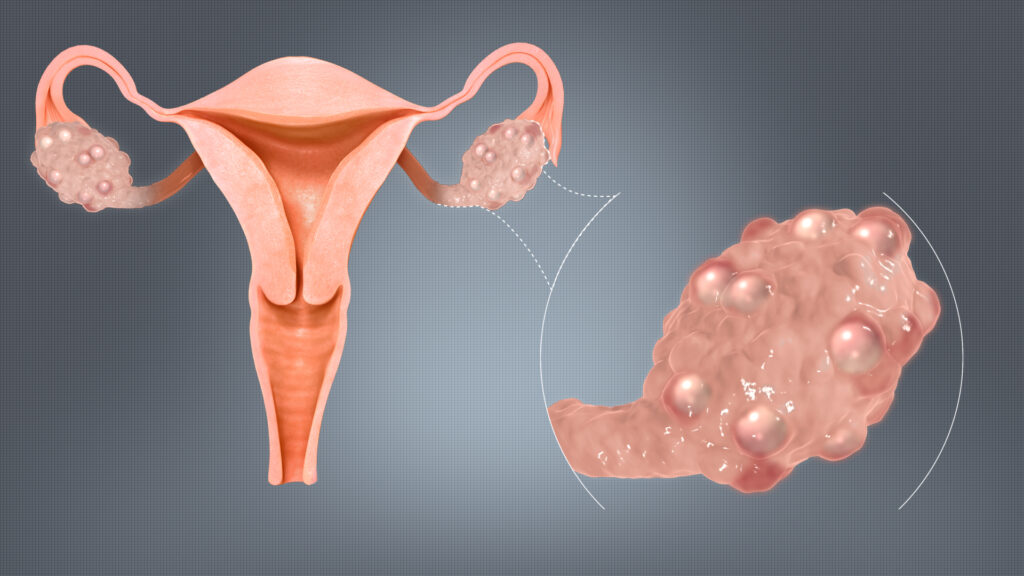
Polycystic ovarian syndrome (PCOS) is a complex endocrine disorder affecting women of reproductive age. It is characterized by hormonal imbalances, irregular ovulation, and the presence of multiple small cysts in the ovaries. PCOS is a leading cause of infertility and is frequently associated with insulin resistance, obesity, and androgen excess.
Key Diagnostic Criteria
The Rotterdam Criteria are widely accepted for PCOS diagnosis. A patient must meet at least two out of the following three conditions:
- Oligo- or anovulation (infrequent or absent ovulation)
- Clinical or biochemical signs of hyperandrogenism (e.g., acne, hirsutism, elevated testosterone)
- Polycystic ovaries on ultrasound (12 or more follicles in each ovary or increased ovarian volume)
These criteria help distinguish PCOS from other endocrine disorders with overlapping features.
Underlying Causes of PCOS
The exact etiology of PCOS is multifactorial and involves complex interactions between genetic, hormonal, and environmental factors. The syndrome often runs in families and is exacerbated by poor lifestyle choices and metabolic dysfunction.
Major Contributing Factors:
- Insulin resistance: A key driver of hyperandrogenism and ovulatory dysfunction
- Increased luteinizing hormone (LH): Stimulates ovarian androgen production
- Low sex hormone-binding globulin (SHBG): Increases free circulating androgens
- Chronic inflammation: Elevates androgen levels and impairs ovarian function
Common Symptoms of Polycystic Ovarian Syndrome
PCOS manifests through a broad range of reproductive, metabolic, and dermatologic symptoms. The presentation may vary, making early diagnosis challenging.
Primary symptoms include:
- Irregular or absent menstrual periods
- Excess facial and body hair (hirsutism)
- Acne and oily skin
- Thinning scalp hair (androgenic alopecia)
- Weight gain or difficulty losing weight
- Infertility due to anovulation
- Mood swings and depression
Long-Term Health Risks
If left untreated, PCOS can lead to serious long-term complications, including:
- Type 2 diabetes mellitus
- Cardiovascular disease
- Endometrial hyperplasia and cancer
- Non-alcoholic fatty liver disease (NAFLD)
- Sleep apnea
- Metabolic syndrome
Diagnostic Procedures and Laboratory Assessment
A thorough diagnosis involves a combination of clinical evaluation, laboratory testing, and imaging.
Hormonal and Biochemical Tests:
- Total and free testosterone
- LH/FSH ratio (typically elevated LH)
- Prolactin and thyroid-stimulating hormone (TSH)
- Glucose tolerance test (OGTT)
- Fasting insulin and lipid profile
Imaging Studies:
- Transvaginal ultrasound: Reveals enlarged ovaries with multiple small follicles arranged peripherally
Advanced PCOS Treatment Options
Effective management of PCOS requires an individualized, multidisciplinary approach targeting both hormonal imbalance and metabolic dysfunction.
1. Lifestyle Modification
Weight loss of just 5-10% can significantly improve insulin sensitivity and restore ovulation. Recommendations include:
- Low-glycemic index (GI) diet
- Regular aerobic and resistance training
- Adequate sleep and stress management
2. Pharmacologic Therapies
For Menstrual Irregularities and Hyperandrogenism:
- Combined oral contraceptives (COCs): Regulate cycles and reduce androgen levels
- Anti-androgens (spironolactone, finasteride): Address hirsutism and acne
- Eflornithine cream: Reduces facial hair growth
For Insulin Resistance:
- Metformin: Improves insulin sensitivity, assists with weight loss, and restores ovulation
For Fertility:
- Letrozole (first-line): Aromatase inhibitor that induces ovulation
- Clomiphene citrate: Selective estrogen receptor modulator
- Gonadotropins or IVF: For resistant or advanced cases
3. Surgical Interventions
- Ovarian drilling: Minimally invasive procedure that may restore ovulation in clomiphene-resistant PCOS
Fertility and PCOS: Navigating Conception Challenges
Women with PCOS often struggle with ovulatory infertility. Timely intervention can lead to successful pregnancies with appropriate treatment protocols.
Optimizing Fertility:
- Monitor ovulation through basal body temperature or LH kits
- Weight loss and diet optimization
- Ovulation induction medications as needed
- Assisted reproductive technologies (ART) when indicated
PCOS and Mental Health: A Holistic Concern
The chronic nature of PCOS, along with its visible symptoms, significantly impacts mental well-being. Studies have shown a higher prevalence of:
- Depression and anxiety
- Body image dissatisfaction
- Eating disorders
Holistic management includes psychological counseling and community support groups.
PCOS in Adolescents: Early Identification Is Key
Adolescents may show early signs of PCOS shortly after menarche. However, diagnosis can be complex due to the natural irregularity of early menstrual cycles. Features requiring evaluation include:
- Persistent acne unresponsive to treatment
- Excessive facial or body hair
- Irregular menses beyond two years post-menarche
- Obesity or rapid weight gain
Early diagnosis can prevent progression to metabolic disease and fertility issues.
PCOS and Skin Manifestations
Androgen excess contributes to several dermatologic symptoms:
- Acne vulgaris: Common, especially along the jawline
- Seborrhea: Oily skin
- Hirsutism: Excess hair on face, chest, back
- Acanthosis nigricans: Dark, velvety skin patches on neck, underarms, groin (marker of insulin resistance)
Monitoring and Follow-Up
Lifelong monitoring is essential for patients with PCOS. Regular assessments should include:
- Annual glucose and lipid testing
- Endometrial surveillance in cases of prolonged amenorrhea
- Monitoring for hypertension and cardiovascular risk
- Bone density evaluations if amenorrhea persists
Polycystic ovarian syndrome is a multifaceted condition with reproductive, metabolic, and psychological dimensions. With early diagnosis, tailored therapy, and lifestyle adjustments, women with PCOS can achieve hormonal balance, improved fertility, and long-term health. Proactive management and continuous patient education are pivotal in minimizing complications and enhancing quality of life.