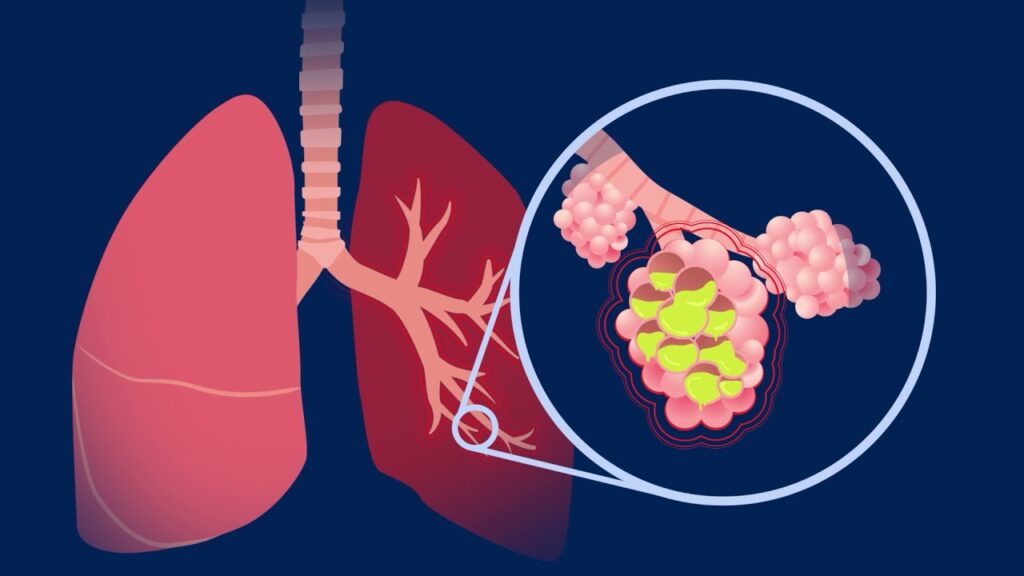
Pneumococcal pneumonia is an acute lower respiratory tract infection caused by Streptococcus pneumoniae, a leading bacterial pathogen responsible for significant global morbidity and mortality. This form of pneumonia primarily affects the lungs and is characterized by rapid symptom onset, alveolar inflammation, and potential systemic complications if not promptly managed. It remains a critical public health concern, particularly among the elderly, immunocompromised individuals, and unvaccinated populations.
Causative Organism: Streptococcus pneumoniae
Streptococcus pneumoniae is a gram-positive, encapsulated diplococcus known for its ability to evade the host immune system through its polysaccharide capsule. It colonizes the nasopharynx asymptomatically but can invade the lower respiratory tract under favorable conditions such as weakened immunity, viral co-infections, or chronic illnesses.
This pathogenic pathway leads to the hallmark features of bacterial pneumonia, including lobar consolidation, hypoxia, and systemic inflammatory symptoms.
Clinical Manifestations of Pneumococcal Pneumonia
The presentation of pneumococcal pneumonia is typically acute and severe, marked by both respiratory and systemic symptoms.
Primary Respiratory Symptoms:
- Productive cough with rust-colored or purulent sputum
- Dyspnea (shortness of breath)
- Pleuritic chest pain
- Tachypnea and respiratory distress
Systemic Signs:
- High-grade fever with chills and rigors
- Fatigue and malaise
- Sweating and myalgia
- Confusion or altered mental status in older adults
Physical examination often reveals:
- Dullness to percussion over the affected lobe
- Bronchial breath sounds
- Crackles and egophony on auscultation
Risk Factors and Susceptible Populations
While pneumococcal pneumonia can affect individuals of any age, several groups are at elevated risk:
- Adults ≥ 65 years
- Infants and children under 2 years
- People with chronic illnesses (e.g., COPD, diabetes, heart disease)
- Immunocompromised individuals (e.g., HIV, cancer patients, transplant recipients)
- Smokers and alcoholics
- Residents of long-term care facilities
Diagnostic Approach and Laboratory Evaluation
A prompt and accurate diagnosis is essential to initiate appropriate antibiotic therapy and reduce mortality.
Diagnostic Tools:
- Chest Radiography (X-ray): Confirms presence of lobar consolidation or infiltrates.
- Sputum Gram Stain and Culture: Identifies gram-positive diplococci and determines antibiotic susceptibility.
- Blood Cultures: Essential in severe cases or suspected bacteremia.
- Urinary Antigen Test for S. pneumoniae: Rapid and specific for pneumococcal antigen detection.
- Complete Blood Count (CBC): Typically reveals leukocytosis with left shift.
- Arterial Blood Gas (ABG): Assesses hypoxemia in critically ill patients.
- CRP and Procalcitonin: Useful markers for bacterial infection and therapeutic monitoring.
Radiological Findings in Pneumococcal Pneumonia
Radiographs typically reveal a well-demarcated area of consolidation in one lobe (lobar pneumonia), most commonly the right lower lobe. Pleural effusions may also be observed in complicated cases.
Management and Antibiotic Therapy
Effective treatment involves the timely initiation of empiric and then targeted antibiotic therapy, based on local resistance patterns and disease severity.
First-Line Antibiotics:
- Amoxicillin (High Dose): Preferred for uncomplicated outpatient cases
- Ceftriaxone or Cefotaxime: Recommended for hospitalized patients
- Levofloxacin or Moxifloxacin: Fluoroquinolones effective for patients with penicillin allergy or in regions with high resistance
Adjunctive Therapy:
- Oxygen supplementation for hypoxia
- Antipyretics for fever and discomfort
- IV fluids for dehydration
- Mechanical ventilation in severe or ICU cases
Treatment Duration:
- Uncomplicated cases: 5–7 days
- Severe cases or bacteremia: 10–14 days
Follow-Up:
Repeat chest X-rays are not routinely required unless clinical deterioration or lack of resolution is noted.
Complications of Untreated or Severe Pneumococcal Pneumonia
Delayed or inadequate treatment can result in life-threatening complications:
- Pleural effusion or empyema
- Lung abscess
- Bacteremia and sepsis
- Meningitis
- Respiratory failure
- Death, particularly in elderly or immunocompromised patients
Prevention Strategies and Vaccination Guidelines
Vaccination remains the cornerstone of pneumococcal disease prevention, especially among high-risk populations.
Recommended Vaccines:
- PCV13 (13-valent pneumococcal conjugate vaccine): For children, adults with comorbidities, and those ≥ 65
- PCV15 and PCV20: Newer conjugate vaccines offering broader protection
- PPSV23 (23-valent polysaccharide vaccine): Recommended for adults ≥ 65 and those with chronic illnesses
Other Preventive Measures:
- Annual influenza vaccination to reduce co-infection risk
- Smoking cessation
- Proper hand hygiene
- Early treatment of respiratory infections
Global Burden and Epidemiology
Pneumococcal pneumonia accounts for a significant proportion of community-acquired pneumonia (CAP) cases worldwide. According to WHO estimates, pneumococcal disease causes over 300,000 deaths annually among adults over 70 and children under five. Vaccine implementation programs have dramatically reduced incidence in many countries, yet gaps in adult vaccination remain.
Antimicrobial Resistance and Surveillance
The emergence of drug-resistant S. pneumoniae strains poses a major clinical challenge. Resistance to penicillin, macrolides, and fluoroquinolones is rising, emphasizing the importance of antimicrobial stewardship and vaccine coverage expansion.
Resistance patterns vary geographically, necessitating regional susceptibility data to inform empiric therapy.
Frequently Asked Questions
What is pneumococcal pneumonia?
It is a lung infection caused by Streptococcus pneumoniae, leading to symptoms such as fever, cough, chest pain, and shortness of breath.
How is pneumococcal pneumonia different from other pneumonias?
It presents more acutely, often with lobar consolidation, and is caused by a specific bacterial pathogen with distinct vaccine-preventable strains.
Is pneumococcal pneumonia contagious?
Yes, it spreads via respiratory droplets, particularly in crowded environments or among close contacts.
Can pneumococcal pneumonia be cured?
Yes, with timely antibiotic treatment, most cases resolve completely, though severe infections may require hospitalization.
Who should get the pneumococcal vaccine?
Children under five, adults over 65, and individuals with chronic health conditions or weakened immunity.
What are the long-term effects of pneumococcal pneumonia?
While most recover fully, some may develop lung scarring, decreased lung function, or suffer recurrent infections if not fully treated.