Pneumococcal infection is caused by Streptococcus pneumoniae, a gram-positive bacterium that can lead to a broad range of illnesses, ranging from mild respiratory conditions to life-threatening invasive diseases. This pathogen is responsible for high global morbidity and mortality, particularly among children under five, the elderly, and immunocompromised individuals.
Types of Pneumococcal Disease
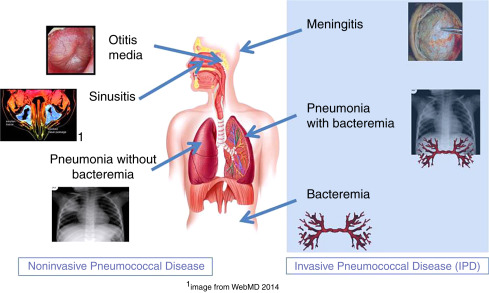
Pneumococcal infections are classified into non-invasive and invasive pneumococcal diseases (IPD):
Non-Invasive Pneumococcal Diseases
- Otitis media: Middle ear infection, especially in children
- Sinusitis: Infection of the paranasal sinuses
- Non-bacteremic pneumonia: Pneumonia not associated with bloodstream infection
Invasive Pneumococcal Diseases (IPD)
- Bacteremic pneumonia: Pneumonia with bacteria present in the blood
- Sepsis: A systemic, life-threatening infection
- Meningitis: Infection of the membranes surrounding the brain and spinal cord
Pathogenesis: How Streptococcus pneumoniae Causes Infection
S. pneumoniae colonizes the nasopharynx asymptomatically in many individuals. However, under conditions such as viral infection, weakened immunity, or mucosal disruption, the bacterium may migrate to normally sterile areas like the lungs, bloodstream, or cerebrospinal fluid, triggering a strong inflammatory response.
Virulence factors include:
- Capsular polysaccharide: Protects against phagocytosis
- Pneumolysin: Cytotoxin that damages host tissues
- Autolysin: Facilitates bacterial lysis and release of inflammatory substances
- Adhesins: Promote attachment to host epithelial cells
Epidemiology and Risk Factors
Global Burden
Pneumococcal infection remains a leading cause of vaccine-preventable deaths, particularly in low- and middle-income countries. Each year, it is estimated to cause:
- ~1 million deaths in children under 5
- ~150,000 hospitalizations in the elderly in developed countries
High-Risk Groups
- Children under 2 years
- Adults ≥65 years
- Individuals with:
- Chronic heart, lung, or liver disease
- Diabetes mellitus
- Immunosuppression (e.g., HIV, chemotherapy)
- Cochlear implants or CSF leaks
- Sickle cell disease or asplenia
- Smoking history
Symptoms of Pneumococcal Infections
Pneumococcal Pneumonia
- Sudden onset of fever, chills
- Cough with rusty or purulent sputum
- Chest pain, shortness of breath
- Confusion in elderly patients
Pneumococcal Meningitis
- High fever
- Neck stiffness
- Photophobia
- Altered mental status
- Seizures
Bacteremia/Sepsis
- Hypotension
- Rapid heart rate
- Cold extremities
- Multi-organ dysfunction
Diagnostic Techniques for Pneumococcal Infection
Laboratory and Imaging
- Blood culture: Confirms bacteremia
- Sputum culture: Identifies causative organism
- Chest X-ray: Evaluates pneumonia
- Lumbar puncture: Essential in suspected meningitis
- Urinary antigen test: Detects pneumococcal polysaccharide
Rapid Tests
- PCR and antigen detection assays enhance sensitivity in identifying S. pneumoniae, especially in culture-negative cases.
Antibiotic Treatment and Resistance Concerns
First-Line Treatment
- Penicillin and amoxicillin remain effective for many strains
- Ceftriaxone or cefotaxime for severe infections
- Vancomycin in penicillin-resistant cases or meningitis
- Macrolides (e.g., azithromycin) for outpatient therapy or in β-lactam allergic individuals
Antimicrobial Resistance
Rising resistance to penicillin and macrolides has been reported globally, primarily due to overuse of antibiotics. Susceptibility testing is essential to guide therapy.
Prevention Through Vaccination
Vaccination remains the most effective method for reducing disease burden.
Pneumococcal Conjugate Vaccine (PCV13, PCV15, PCV20)
- Covers most common invasive serotypes
- Administered in early childhood (2, 4, 6, and 12–15 months)
- Also recommended for adults ≥65 and high-risk groups
Pneumococcal Polysaccharide Vaccine (PPSV23)
- Broader serotype coverage
- Used primarily in adults and those with chronic illnesses
Combined Vaccination Strategy
- Adults ≥65 or immunocompromised should receive both PCV and PPSV with appropriate spacing.
Public Health Impact of Pneumococcal Vaccination
Since the introduction of routine pneumococcal immunization:
- There has been a significant decline in invasive disease rates, especially in children.
- Herd immunity has provided indirect protection to unvaccinated individuals.
- Serotype replacement (non-vaccine serotypes becoming more prevalent) is an emerging challenge.
Complications and Long-Term Effects
If untreated or inadequately managed, pneumococcal infections may lead to:
- Hearing loss (post-meningitis)
- Brain damage
- Chronic lung conditions
- Death, particularly in vulnerable populations
Early intervention and supportive care are essential for improving outcomes.
Strategies for Reducing Pneumococcal Disease Burden
- Universal vaccination programs
- Public awareness campaigns
- Reducing antibiotic misuse
- Strengthening healthcare systems in low-resource settings
- Surveillance systems for tracking serotype shifts and resistance
Pneumococcal infection remains a formidable global health concern with serious clinical consequences, particularly in children, the elderly, and immunocompromised individuals. Advances in vaccination have significantly reduced the burden, but ongoing surveillance, responsible antibiotic use, and public health initiatives are essential to sustain progress and adapt to emerging challenges.