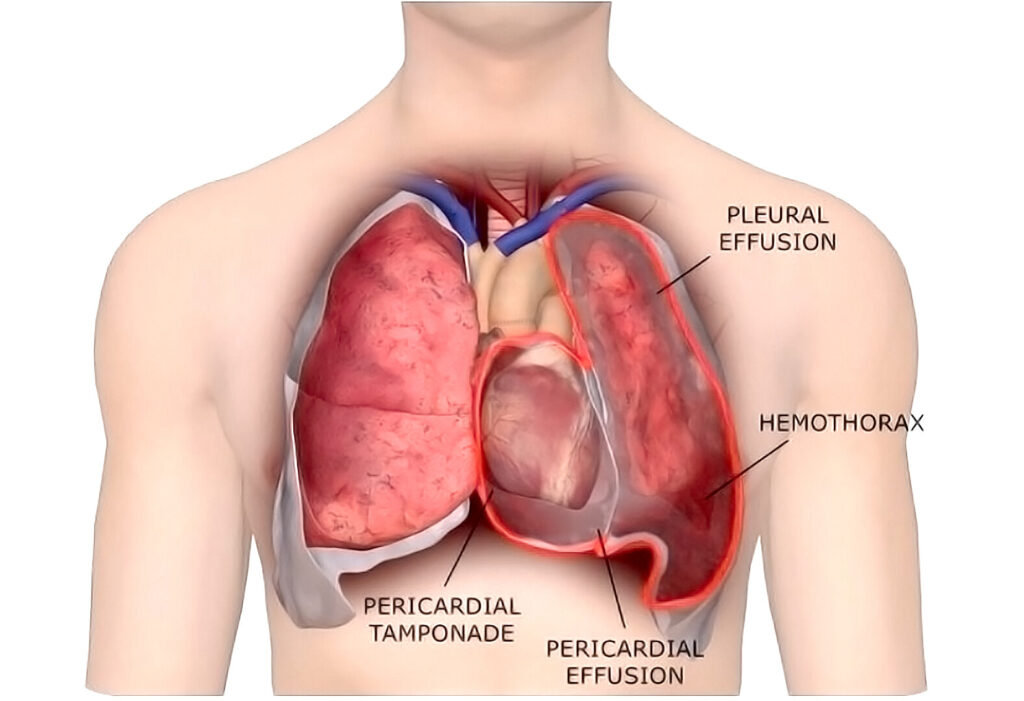
Malignant pleural effusion (MPE) is a serious oncologic condition characterized by the abnormal accumulation of cancer-related fluid in the pleural cavity. This condition typically indicates advanced malignancy and is associated with poor prognosis. It severely impacts respiratory function and quality of life, necessitating timely and strategic intervention.
Pathophysiology of Malignant Pleural Effusion
MPE results from metastatic involvement of the pleura, which disrupts the balance between fluid production and absorption. Tumor infiltration leads to increased vascular permeability and obstruction of lymphatic drainage, causing fluid accumulation.
Malignant cells in the pleural space release cytokines and growth factors that further exacerbate fluid retention and inflammation.
Common Cancers Associated with MPE
The majority of malignant pleural effusions are secondary to metastatic cancers. Primary sites include:
- Lung cancer (most frequent cause)
- Breast cancer
- Lymphomas
- Ovarian cancer
- Gastrointestinal cancers
- Mesothelioma (primary pleural malignancy)
Clinical Presentation of Malignant Pleural Effusion
Symptoms develop progressively and are often indicative of underlying cancer progression. The key clinical features include:
- Shortness of breath, especially on exertion
- Non-productive cough
- Chest pain, often pleuritic in nature
- Fatigue and weight loss
- Orthopnea (in large effusions)
- Dullness to percussion and decreased breath sounds on examination
MPE can be recurrent and refractory to simple fluid drainage, highlighting the need for definitive management.
Diagnostic Evaluation of Malignant Pleural Effusion
Imaging Modalities
- Chest X-ray: Initial assessment showing unilateral or bilateral effusions.
- Ultrasound: Determines effusion volume and guides thoracentesis.
- CT Scan: Reveals pleural thickening, nodularity, and mediastinal involvement.
Diagnostic Thoracentesis
Pleural fluid analysis remains the cornerstone of diagnosis.
Pleural Fluid Characteristics:
- Exudative by Light’s criteria
- Elevated LDH and protein levels
- Low glucose and pH in some cases
- Malignant cytology: Identification of cancer cells confirms the diagnosis in ~60% of cases
- Flow cytometry: Especially useful in hematologic malignancies
Pleural Biopsy
When cytology is inconclusive, pleural biopsy is essential:
- Image-guided needle biopsy
- Thoracoscopic (VATS) biopsy for direct visualization and tissue sampling
Treatment Strategies for Malignant Pleural Effusion
The goals of MPE treatment are symptom relief, recurrence prevention, and enhancement of patient comfort. The approach depends on the patient’s performance status, expected survival, and the nature of the effusion.
Therapeutic Thoracentesis
- Provides immediate symptomatic relief
- Appropriate for small, non-recurrent effusions
- Repeated thoracenteses may be necessary in recurrent MPE but carry the risk of infection and pneumothorax
Chest Tube Drainage with Chemical Pleurodesis
- Pleurodesis: Obliteration of the pleural space by instilling sclerosing agents (e.g., talc) through a chest tube
- High success rate (~70–90%) in preventing recurrence
- Ideal for patients with expandable lung and longer expected survival
Indwelling Pleural Catheters (IPC)
- Tunnelled pleural catheters enable intermittent outpatient drainage
- Improves quality of life and minimizes hospital stays
- Suitable for patients unfit for pleurodesis or with trapped lung
- Potential complications: infection, catheter blockage
Surgical Interventions
- Video-Assisted Thoracoscopic Surgery (VATS): Facilitates talc poudrage pleurodesis or pleurectomy
- Reserved for patients with good performance status and recurrent, symptomatic effusion
- Allows simultaneous biopsy for histological confirmation
Prognosis and Survival Outcomes
Malignant pleural effusion is a marker of advanced-stage cancer and correlates with limited life expectancy. Median survival varies based on the primary tumor:
- Lung cancer: 3–6 months
- Breast cancer: 6–12 months
- Lymphoma: >12 months in responsive disease
- Mesothelioma: Variable; dependent on subtype and response to treatment
Early diagnosis and palliative interventions can greatly improve functional status and patient comfort.
Preventing Recurrence of MPE
To reduce recurrence, pleurodesis and indwelling pleural catheters are primary modalities. Patient-specific strategies include:
- Timely initiation of systemic cancer therapy
- Minimizing delays in drainage or catheter placement
- Multidisciplinary coordination between oncology, pulmonology, and palliative care
Malignant pleural effusion is a serious complication of advanced cancers that significantly impairs respiratory function and quality of life. An accurate and swift diagnostic approach followed by patient-tailored management—ranging from thoracentesis and pleurodesis to surgical procedures—is vital for optimal outcomes. The integration of palliative care principles ensures dignity and comfort in advanced stages of disease.