Plasmodium ovale is one of the five species of Plasmodium known to cause malaria in humans. Though less prevalent than P. falciparum or P. vivax, P. ovale is medically significant due to its potential for relapse and its ability to persist in the liver in a dormant form known as the hypnozoite. This article provides an extensive overview of Plasmodium ovale malaria, covering its epidemiology, clinical features, diagnostic methods, treatment protocols, and preventive strategies.
Epidemiology of Plasmodium ovale Malaria
Plasmodium ovale is geographically limited but often underreported due to diagnostic challenges.
- Geographic Distribution: Most commonly found in Sub-Saharan Africa, Papua New Guinea, and parts of Southeast Asia.
- Prevalence: Rare compared to P. falciparum and P. vivax, accounting for less than 5% of malaria cases globally.
- Co-infection: Often occurs alongside other Plasmodium species, complicating clinical presentation and diagnosis.
Lifecycle and Transmission of Plasmodium ovale
Understanding the parasite’s lifecycle is essential for designing effective control and treatment measures.
Transmission via Anopheles Mosquito
- The disease is transmitted by the bite of an infected female Anopheles mosquito.
- Sporozoites enter the human bloodstream and invade liver cells, initiating the exoerythrocytic cycle.
Dormancy and Relapse
- Like P. vivax, P. ovale can form dormant liver stages (hypnozoites).
- These hypnozoites can reactivate weeks to months after the initial infection, causing relapse.
Clinical Features and Symptoms of Ovale Malaria
Symptoms of P. ovale infection are generally mild to moderate but can become severe if left untreated.
Common Symptoms
- Intermittent fever (every 48 hours)
- Chills, headache, muscle aches
- Nausea, vomiting, and fatigue
- Enlarged spleen and mild anemia
Relapsing Nature
- Relapses may mimic new infections and delay complete recovery.
- In non-endemic travelers, relapses can occur long after returning from a malaria-endemic area.
Diagnostic Methods for Plasmodium ovale Malaria
Accurate diagnosis is often delayed or missed due to morphological similarities with other species.
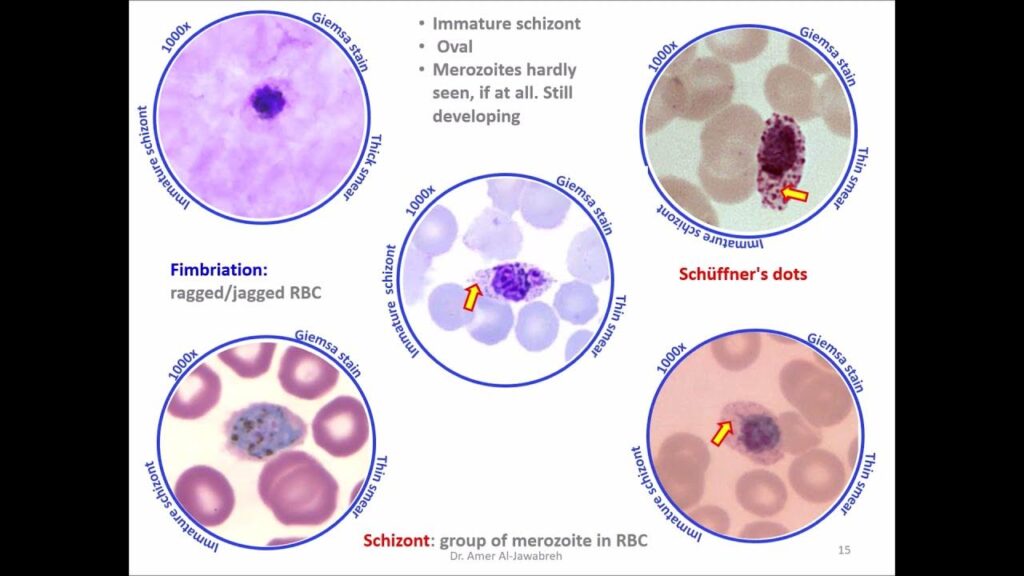
Microscopic Examination
- Blood smear microscopy remains the gold standard.
- P. ovale trophozoites and schizonts can resemble P. vivax but tend to be more compact with fimbriated edges.
Rapid Diagnostic Tests (RDTs)
- Most RDTs are optimized for P. falciparum and P. vivax, with lower sensitivity for P. ovale.
Molecular Diagnostics
- Polymerase Chain Reaction (PCR) offers high specificity and is ideal for detecting mixed infections or low-level parasitemia.
Treatment Protocols for Ovale Malaria
Effective treatment requires targeting both blood-stage parasites and dormant liver stages.
First-Line Antimalarial Therapy
- Chloroquine remains effective for treating blood stages of P. ovale.
- Artemisinin-based combination therapies (ACTs) may be used where resistance or mixed infections are suspected.
Radical Cure with Primaquine
- Primaquine is necessary to eliminate liver-stage hypnozoites and prevent relapse.
- A G6PD deficiency test must be conducted prior to administration due to the risk of hemolytic anemia.
Prevention Strategies for Plasmodium ovale Malaria
Prevention hinges on avoiding mosquito bites and managing potential relapse through chemoprophylaxis.
Personal Protection Measures
- Use of long-lasting insecticide-treated nets (LLINs)
- Wearing protective clothing during evening hours
- Application of DEET-based mosquito repellents
- Use of indoor residual spraying (IRS) in endemic regions
Chemoprophylaxis for Travelers
- Atovaquone-proguanil, doxycycline, or mefloquine may be recommended based on regional resistance patterns.
- Terminal prophylaxis with primaquine is advised for travelers to areas where P. ovale is prevalent, especially after return.
Public Health Importance and Control Challenges
Asymptomatic Carriers
- Individuals may carry the parasite without showing symptoms, serving as reservoirs for transmission.
Surveillance and Reporting
- Accurate data collection and reporting are essential to understanding the true burden of P. ovale malaria.
- Inclusion in national malaria control programs is often insufficient, hampering elimination efforts.
FAQs:
Q1: What makes Plasmodium ovale different from other malaria species?
Plasmodium ovale is notable for its ability to form hypnozoites, causing relapses months after the initial infection.
Q2: Is P. ovale malaria fatal?
Though generally mild, it can be dangerous if untreated, especially in immunocompromised individuals or those with co-infections.
Q3: Can standard malaria tests detect P. ovale?
Not reliably. Microscopy and molecular tests like PCR are more accurate than rapid diagnostic tests for detecting P. ovale.
Q4: How long after travel can P. ovale malaria relapse?
Relapse can occur up to several months, even a year, after exposure due to the hypnozoite stage in the liver.
Q5: Is there a vaccine for Plasmodium ovale?
Currently, there is no vaccine specifically targeting P. ovale. Vaccine development remains focused on P. falciparum.
Plasmodium ovale malaria, though often overshadowed by more virulent species, remains a challenge in malaria control and elimination efforts due to its capacity for relapse and underdiagnosis. Through effective diagnostics, appropriate treatment regimens, personal protection, and strengthened public health strategies, we can mitigate the spread and burden of this often-overlooked form of malaria.