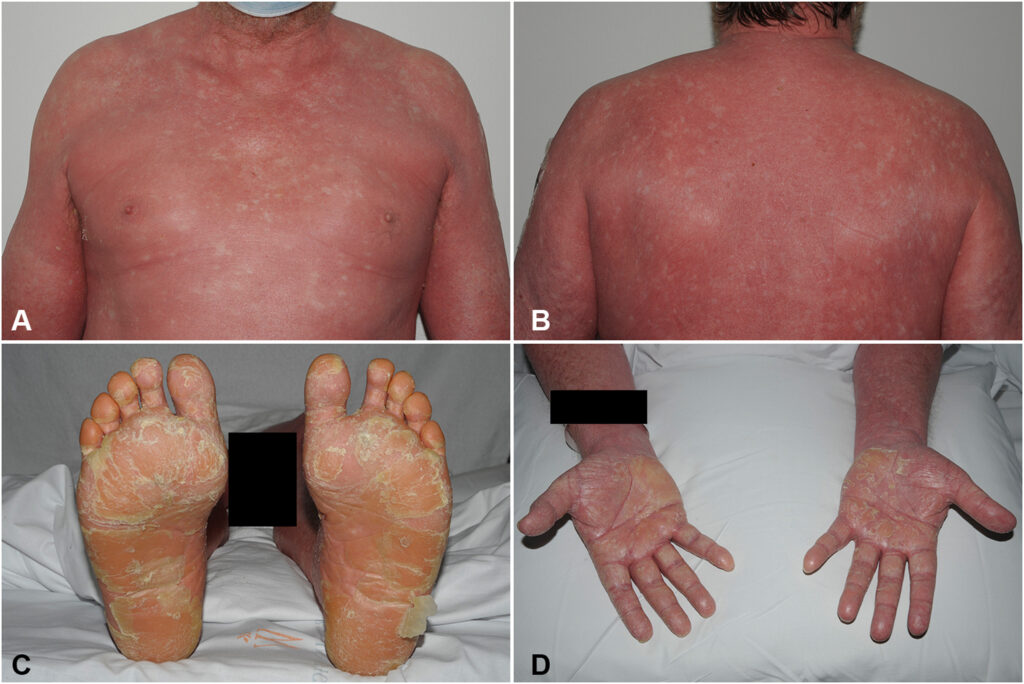
Pityriasis rubra pilaris (PRP) is a rare, chronic dermatologic condition characterized by follicular hyperkeratosis, erythroderma, and palmoplantar keratoderma. The disease often progresses from isolated patches of rough, scaly skin to widespread involvement, sometimes affecting the entire body. While PRP can occur at any age, it presents with distinct clinical features based on age of onset and subtype.
Understanding the Pathogenesis of Pityriasis Rubra Pilaris
The pathophysiology of PRP is not fully understood. However, it is believed to involve disruption of epidermal differentiation and keratinization. Recent studies suggest genetic mutations, particularly in the CARD14 gene, may play a role, especially in familial forms. The disease is thought to result from an abnormal immune response, leading to excessive inflammation and skin turnover.
Clinical Features and Symptoms of PRP Skin Disease
PRP typically presents with a progressive skin rash, which evolves in distinct phases and patterns:
- Follicular keratotic papules: Rough, red, cone-shaped papules that cluster around hair follicles.
- Waxy, yellow-orange scaling plaques: Often found on elbows, knees, and scalp.
- Widespread erythema: Diffuse redness may progress to erythroderma in severe cases.
- Palmoplantar keratoderma: Thickened, orange-hued skin on the palms and soles.
- “Islands of sparing”: Areas of unaffected skin amid erythroderma, a hallmark of PRP.
- Pruritus: Itching varies by patient and disease severity.
- Nail changes: Thickening, ridging, and discoloration can occur.
- Hair loss: Scalp involvement may lead to alopecia.
Classification: Types of Pityriasis Rubra Pilaris
PRP is categorized into six distinct types based on age of onset, distribution, and clinical progression:
| Type | Description | Onset | Features |
|---|---|---|---|
| Type I | Classic Adult | Most common (55%) | Widespread erythema, palmoplantar keratoderma, islands of sparing |
| Type II | Atypical Adult | Chronic course | Ichthyosiform scaling, eczematous features, alopecia |
| Type III | Classic Juvenile | Childhood | Similar to Type I, often follows infections |
| Type IV | Circumscribed Juvenile | Localized | Elbows, knees, palmoplantar hyperkeratosis |
| Type V | Atypical Juvenile | Early onset | Familial, CARD14 mutations, chronic |
| Type VI | HIV-associated | Associated with immunosuppression | Poor response to therapy, extensive scaling |
Causes and Risk Factors
While the exact cause of PRP remains idiopathic, multiple factors have been implicated:
- Genetic predisposition: Mutations in the CARD14 gene, especially in familial (Type V) PRP.
- Autoimmune or inflammatory triggers
- Viral infections: Including HIV, linked with Type VI.
- Drug reactions: Rarely, PRP has occurred following certain medications.
- Environmental factors: Cold climates may worsen the condition.
Diagnosis of Pityriasis Rubra Pilaris
The diagnosis is primarily clinical, supported by histopathologic findings.
Clinical Diagnosis
Dermatologists rely on the distinctive triad:
- Follicular papules
- Orange-salmon colored plaques
- Palmoplantar keratoderma with islands of sparing
Skin Biopsy and Histology
Histopathologic features include:
- Alternating orthokeratosis and parakeratosis in vertical and horizontal patterns.
- Follicular plugging
- Irregular acanthosis
- Sparse superficial perivascular lymphocytic infiltrate
These features help distinguish PRP from psoriasis, which it often mimics in early stages.
Differential Diagnosis
Accurate differentiation is essential to avoid misdiagnosis. Conditions that resemble PRP include:
- Psoriasis vulgaris
- Seborrheic dermatitis
- Atopic dermatitis
- Ichthyosis vulgaris
- Cutaneous T-cell lymphoma (CTCL)
Treatment Options for Pityriasis Rubra Pilaris
Management of PRP can be complex due to its variable course and therapeutic response. Treatment is typically individualized based on type and severity.
1. Topical Therapies
- Emollients: Restore skin barrier.
- Keratolytics (salicylic acid, urea): Reduce scaling.
- Topical corticosteroids: Alleviate inflammation.
- Calcipotriol: Vitamin D analog used in mild PRP.
2. Systemic Retinoids
- Acitretin and Isotretinoin: First-line agents.
- Normalize keratinization and reduce scaling.
- Require monitoring of liver function and lipid profiles.
3. Methotrexate
- Immunosuppressive agent used in recalcitrant PRP.
- Effective in adult and HIV-associated cases.
4. Biologic Agents
Emerging options showing promise in resistant cases:
- TNF-alpha inhibitors: Infliximab, etanercept
- IL-12/23 inhibitors: Ustekinumab
- IL-17 inhibitors: Secukinumab
These therapies are especially valuable in Type VI and psoriasiform variants of PRP.
5. Phototherapy
- Narrowband UVB or PUVA: May benefit localized or circumscribed PRP.
- Requires caution due to potential exacerbation in some patients.
Prognosis and Long-Term Management
The course of PRP varies:
- Type I (classic adult) often resolves spontaneously within 3 years.
- Atypical and juvenile types may be chronic and refractory.
- Relapses are common, particularly after treatment discontinuation.
Patients benefit from:
- Regular follow-up
- Psychosocial support
- Treatment of comorbidities, especially in immunosuppressed patients
Living with PRP: Patient Guidance
- Maintain hydrated skin using moisturizers regularly.
- Avoid harsh soaps, heat, and irritants.
- Wear breathable fabrics to reduce discomfort from scaling.
- Monitor for signs of secondary infection or drug side effects.
- Collaborate with dermatologists for tailored care plans.
Pityriasis rubra pilaris is a rare but impactful dermatologic disorder marked by its distinct clinical features and variable progression. Advances in immunopathology and molecular genetics are shaping the future of PRP management, particularly in recalcitrant cases. Early diagnosis, individualized treatment, and long-term care coordination are vital to improving patient outcomes and quality of life.