Pituitary dwarfism, also referred to as growth hormone deficiency (GHD), is a rare condition that results in abnormally short stature due to insufficient production of growth hormone (GH) by the pituitary gland. This endocrine disorder typically presents during childhood and can profoundly affect physical development, though cognitive function usually remains unaffected.
Overview of the Pituitary Gland and Hormonal Role
The pituitary gland, often called the “master gland,” is a pea-sized structure located at the base of the brain. It regulates various endocrine functions by secreting hormones, including GH, which is crucial for normal skeletal and muscular growth during childhood and adolescence.
Primary Functions of Growth Hormone:
- Stimulates long bone growth
- Promotes protein synthesis
- Enhances fat metabolism
- Supports organ development
A deficiency in this hormone leads to pituitary dwarfism, a condition marked by proportional but significantly reduced physical stature.
Causes and Risk Factors of Pituitary Dwarfism
Pituitary dwarfism can arise due to congenital or acquired disruptions in the function of the pituitary gland.
Congenital Causes:
- Genetic mutations (e.g., GH1, PROP1, POU1F1)
- Midline brain defects (e.g., septo-optic dysplasia)
- Pituitary hypoplasia
Acquired Causes:
- Brain tumors affecting the hypothalamus or pituitary (e.g., craniopharyngioma)
- Head trauma
- Radiation therapy
- Central nervous system infections (e.g., meningitis)
Clinical Features and Symptoms of Pituitary Dwarfism
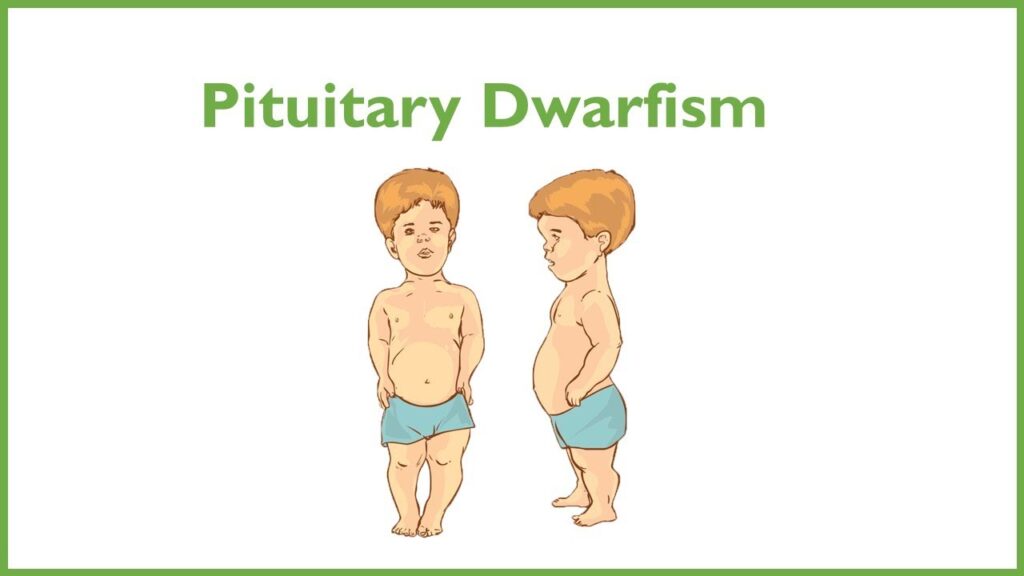
Children with pituitary dwarfism display a pattern of proportionate short stature, with all body parts in scale but significantly below average height for age and sex.
Common Symptoms:
- Height significantly below the 3rd percentile on growth charts
- Slowed or absent growth velocity
- Immature facial appearance
- Delayed puberty
- Increased abdominal fat
- Low muscle tone
- Normal intelligence
In some cases, there may be associated deficiencies in other pituitary hormones, leading to symptoms such as hypothyroidism or adrenal insufficiency.
Diagnosis of Growth Hormone Deficiency
Early and accurate diagnosis is essential for effective intervention. Evaluation involves clinical assessments, growth monitoring, and endocrine testing.
Diagnostic Process:
- Growth Chart Analysis
Repeated measurements reveal growth patterns deviating from expected norms. - Hormonal Assays
- GH stimulation tests (e.g., insulin tolerance test, arginine test)
- Measurement of IGF-1 and IGFBP-3 levels
- Imaging Studies
- MRI of the brain to assess pituitary and hypothalamic structures
- Genetic Testing
Used when a familial or congenital cause is suspected
Differential Diagnosis of Pituitary Dwarfism
Several other conditions may result in short stature and must be differentiated from pituitary dwarfism for precise treatment planning.
Key Conditions to Differentiate:
- Constitutional growth delay
- Familial short stature
- Hypothyroidism
- Turner syndrome
- Chronic systemic illness
- Skeletal dysplasias (e.g., achondroplasia)
Treatment and Management of Pituitary Dwarfism
The primary goal of treatment is to restore growth velocity and help the child achieve a height within the normal adult range. Recombinant human growth hormone (rhGH) therapy is the cornerstone of treatment.
Growth Hormone Therapy:
- Daily subcutaneous injections
- Initiated as early as possible
- Doses adjusted based on weight, age, and response
- Continued until epiphyseal plate closure or desired height is achieved
Monitoring:
- Regular assessment of growth velocity
- Periodic measurement of IGF-1 levels
- MRI follow-up if a tumor was initially identified
Supportive Management:
- Treatment of associated hormone deficiencies
- Nutritional support
- Psychosocial counseling
Prognosis and Long-Term Outlook
With early intervention and proper management, many children with pituitary dwarfism achieve near-normal adult height. However, delayed diagnosis or non-compliance with treatment may result in compromised outcomes.
Long-Term Considerations:
- Lifelong hormone monitoring
- Potential need for continued hormone replacement in adulthood
- Regular endocrinological evaluations
Complications and Associated Conditions
Although GH therapy is generally well-tolerated, certain complications may arise:
- Slipped capital femoral epiphysis
- Increased intracranial pressure
- Hyperglycemia or insulin resistance
- Joint and muscle discomfort
Rarely, benign intracranial hypertension or scoliosis progression may be observed.
Prevention and Genetic Counseling
While congenital pituitary dwarfism cannot be prevented, early detection and prompt therapy can significantly improve quality of life. In cases with a genetic basis, genetic counseling is advised for families planning further pregnancies.
Pituitary dwarfism, a rare but treatable form of short stature, highlights the importance of growth surveillance and early endocrinologic intervention. Advances in GH replacement therapy have transformed the outlook for affected individuals, enabling them to lead healthy, productive lives with normal adult stature. Ongoing research continues to explore optimized therapeutic strategies and deeper genetic insights into this endocrine disorder.