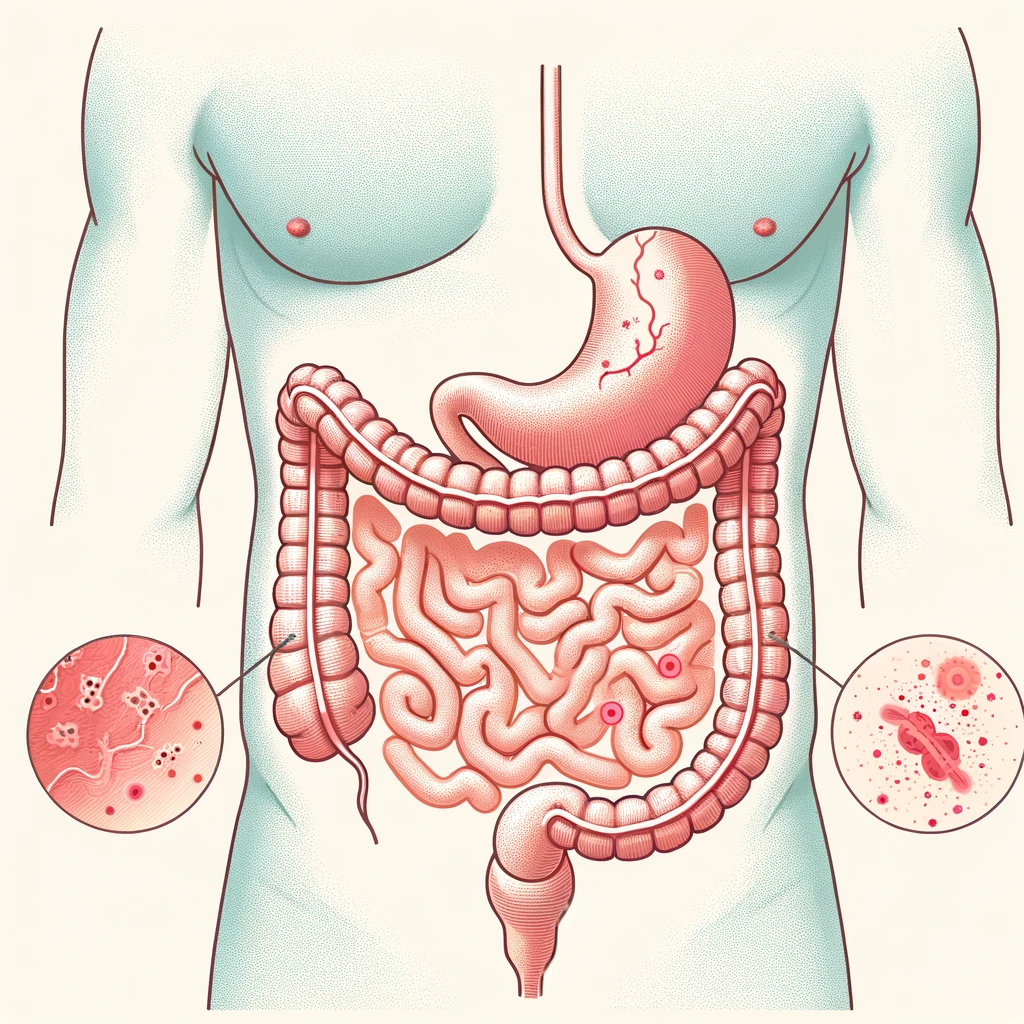
Bacteroides peritonitis is a severe intra-abdominal infection caused by bacteria of the genus Bacteroides. These anaerobic bacteria, particularly Bacteroides fragilis, are part of the normal gut microbiota but can become pathogenic when they escape the gastrointestinal tract. This article delves into the etiology, clinical manifestations, diagnostic methods, treatment approaches, and preventive strategies for managing this condition effectively.
Etiology and Pathogenesis
The Role of Bacteroides in the Human Microbiome
Bacteroides species are gram-negative, obligate anaerobes that predominantly reside in the colon. They play a critical role in maintaining gut homeostasis, aiding in digestion, and regulating the immune response. However, disruptions in the intestinal barrier or surgical interventions can lead to their translocation and subsequent infection.
How Bacteroides Causes Peritonitis
Peritonitis occurs when Bacteroides bacteria gain access to the sterile peritoneal cavity. This can result from:
- Perforated Viscera: Conditions like appendicitis, diverticulitis, or peptic ulcers.
- Trauma or Surgery: Accidental spillage of intestinal contents.
- Peritoneal Dialysis: A complication in patients undergoing continuous ambulatory peritoneal dialysis (CAPD).
Clinical Presentation
Common Symptoms
Patients with Bacteroides peritonitis may present with:
- Severe abdominal pain and tenderness
- Fever and chills
- Nausea and vomiting
- Tachycardia
- Guarding or rigidity of the abdominal wall
Complications
If untreated, the condition can lead to:
- Sepsis
- Multiorgan failure
- Abscess formation
Diagnosis
Laboratory Investigations
- Blood Tests: Elevated white blood cell (WBC) count, C-reactive protein (CRP), and procalcitonin levels.
- Microbial Cultures: Peritoneal fluid samples cultured for aerobic and anaerobic bacteria.
Imaging Studies
- Ultrasound or CT Scan: Identify abscesses, perforations, or free fluid in the abdomen.
- MRI: For detailed imaging in complex cases.
Diagnostic Criteria
A combination of clinical signs, imaging findings, and positive microbial cultures confirms the diagnosis.
Treatment
Antibiotic Therapy
Empirical broad-spectrum antibiotics covering anaerobic bacteria are initiated promptly. Common regimens include:
- Metronidazole: Effective against anaerobes.
- Beta-Lactam/Beta-Lactamase Inhibitors: E.g., piperacillin-tazobactam.
- Carbapenems: E.g., meropenem for severe infections.
Therapy is adjusted based on culture results and antimicrobial susceptibility testing.
Surgical Intervention
- Source Control: Drainage of abscesses or repair of perforated viscera.
- Peritoneal Lavage: Removal of infected material.
Supportive Care
- Intravenous fluids and electrolyte management.
- Monitoring and treating sepsis or organ dysfunction.
Prevention
In Surgical Settings
- Maintain strict asepsis during abdominal surgeries.
- Use prophylactic antibiotics when indicated.
For Peritoneal Dialysis Patients
- Educate on proper catheter care.
- Promptly address signs of infection to prevent complications.
Prognosis
The outcome of Bacteroides peritonitis depends on early diagnosis and appropriate treatment. Mortality rates are significantly higher in delayed or complicated cases, underscoring the importance of timely medical intervention.