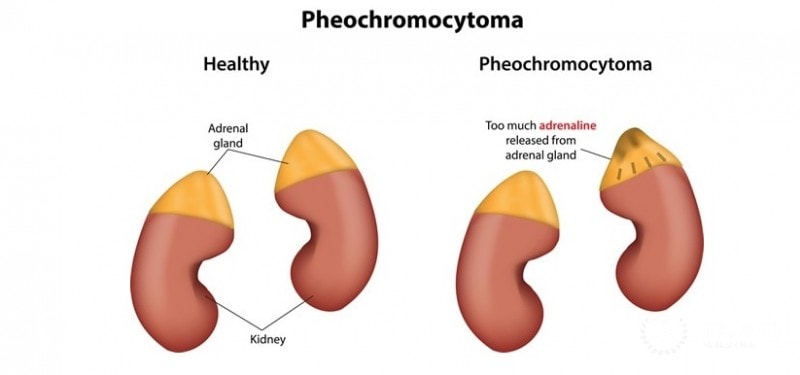
Pheochromocytoma Adjunct Therapy: Pheochromocytoma is a catecholamine-secreting tumor that primarily arises from the adrenal medulla. While surgical resection remains the cornerstone of treatment, adjunct therapies are crucial for managing inoperable, metastatic, or recurrent tumors. These complementary treatments aim to control hormone production, inhibit tumor growth, reduce recurrence, and improve overall survival.
Understanding the Role of Adjunct Therapies in Pheochromocytoma Management
Adjunct therapies are utilized when surgery is not feasible or when malignancy presents with metastatic spread. They complement primary surgical resection by addressing persistent catecholamine excess, treating tumor recurrence, or targeting systemic disease.
Pharmacologic Adjunct Therapy for Symptom Control
Effective medical management is essential in patients awaiting surgery or those with residual disease.
Alpha-Adrenergic Blockade
- Phenoxybenzamine: A non-selective, irreversible alpha-blocker; mitigates hypertension and reduces intraoperative crises.
- Doxazosin, Prazosin: Selective alpha-1 blockers with fewer side effects; often used in outpatient settings.
Beta-Adrenergic Blockade
- Initiated only after alpha blockade to prevent hypertensive emergencies.
- Propranolol, Atenolol, Metoprolol: Control tachyarrhythmias, palpitations, and catecholamine-induced cardiac stress.
Calcium Channel Blockers
- Nifedipine, Amlodipine: Useful for blood pressure control in patients intolerant to alpha-blockers.
Metyrosine (α-Methyltyrosine)
- Inhibits tyrosine hydroxylase, the rate-limiting enzyme in catecholamine biosynthesis.
- Particularly effective in metastatic or unresectable tumors.
- Reduces catecholamine burden and preoperative complication risk.
Radionuclide Therapy: Molecular Targeted Approaches
Iodine-131 Metaiodobenzylguanidine (I-131 MIBG)
- A norepinephrine analog selectively taken up by chromaffin tissue.
- Used in patients with MIBG-avid tumors for symptom palliation and tumor burden reduction.
- Suitable for non-resectable and metastatic pheochromocytomas and paragangliomas.
Benefits:
- Minimally invasive and systemic in action.
- Prolongs progression-free survival.
- Reduces catecholamine-related morbidity.
Limitations:
- Not all tumors are MIBG-avid.
- Requires specialized nuclear medicine facilities.
Peptide Receptor Radionuclide Therapy (PRRT)
- 177Lu-DOTATATE or 90Y-DOTATOC used in tumors expressing somatostatin receptors.
- Especially effective in SDHB-mutated metastatic pheochromocytomas and paragangliomas.
Chemotherapy Regimens for Malignant Pheochromocytoma
Chemotherapy is indicated in progressive, metastatic, or symptomatic malignant cases that do not respond to other treatments.
CVD Regimen
- Cyclophosphamide, Vincristine, Dacarbazine
- Considered the standard chemotherapeutic protocol.
- Produces partial responses and temporary symptom control.
Temozolomide
- An alkylating agent with good central nervous system penetration.
- Preferred in tumors with SDHB mutations due to higher susceptibility.
Emerging Agents
- Research on etoposide, cisplatin, and paclitaxel shows promise in resistant pheochromocytoma lines.
Targeted Therapies and Immunotherapy: Precision Medicine in Action
Tyrosine Kinase Inhibitors (TKIs)
- Sunitinib, Pazopanib: Block angiogenesis by inhibiting VEGFR and PDGFR pathways.
- Beneficial in SDHB-related metastatic tumors.
HIF-2α Inhibitors
- Tumors with VHL mutations often show HIF pathway dysregulation.
- Novel inhibitors under investigation may selectively suppress tumor progression.
mTOR Inhibitors
- Everolimus targets mTOR signaling involved in cellular proliferation and metabolism.
- Under evaluation in multi-drug resistant pheochromocytomas.
Immunotherapy
- Immune checkpoint inhibitors (e.g., anti-PD-1, anti-CTLA-4) are under clinical trials.
- Potential option for advanced pheochromocytomas with high mutational load.
Genetic Counseling and Surveillance
Given the hereditary basis in 30–40% of pheochromocytoma cases, genetic screening informs long-term management and adjunctive therapy choices.
Key Mutations:
- SDHB: Linked with high metastatic risk
- RET: Associated with MEN 2 syndrome
- VHL, NF1, TMEM127, MAX: Require tailored surveillance protocols
Genetic profiling also assists in choosing targeted treatments such as PRRT or TKIs, optimizing adjunct therapy efficacy.
Multimodal Therapy Strategy
A coordinated, multidisciplinary approach improves outcomes in complex pheochromocytoma cases. Integration of surgery, pharmacotherapy, nuclear medicine, oncology, and genetics offers the best survival advantage.
Adjunct therapy in pheochromocytoma represents a crucial dimension in modern oncologic endocrinology. Through a combination of pharmacologic control, radionuclide treatment, chemotherapy, and targeted therapies, we can effectively manage advanced and metastatic disease, improve patient survival, and reduce recurrence. Future innovations, including immunotherapy and gene-targeted drugs, hold significant promise in reshaping pheochromocytoma treatment paradigms.