Pharyngitis Due to Haemophilus parainfluenzae: Haemophilus parainfluenzae is an opportunistic, gram-negative bacterium commonly found in the upper respiratory tract. Though often part of the normal oropharyngeal flora, it has emerged as a significant pathogen implicated in pharyngeal infections. This form of pharyngitis can be clinically indistinguishable from viral or streptococcal pharyngitis, yet requires targeted antimicrobial therapy for resolution.
Pathophysiology of Haemophilus parainfluenzae-Associated Pharyngitis
H. parainfluenzae invades the mucosal lining of the pharynx when host immunity is compromised or when mucosal barriers are disrupted. The bacterium produces proteases and adhesins that facilitate colonization and local inflammation.
Risk Factors for Infection
- Immunocompromised states (e.g., diabetes, cancer)
- Recent upper respiratory viral infection
- Chronic respiratory diseases such as COPD
- Smoking and environmental pollutants
- Prolonged antibiotic use disrupting flora
- Use of corticosteroids or immunosuppressive agents
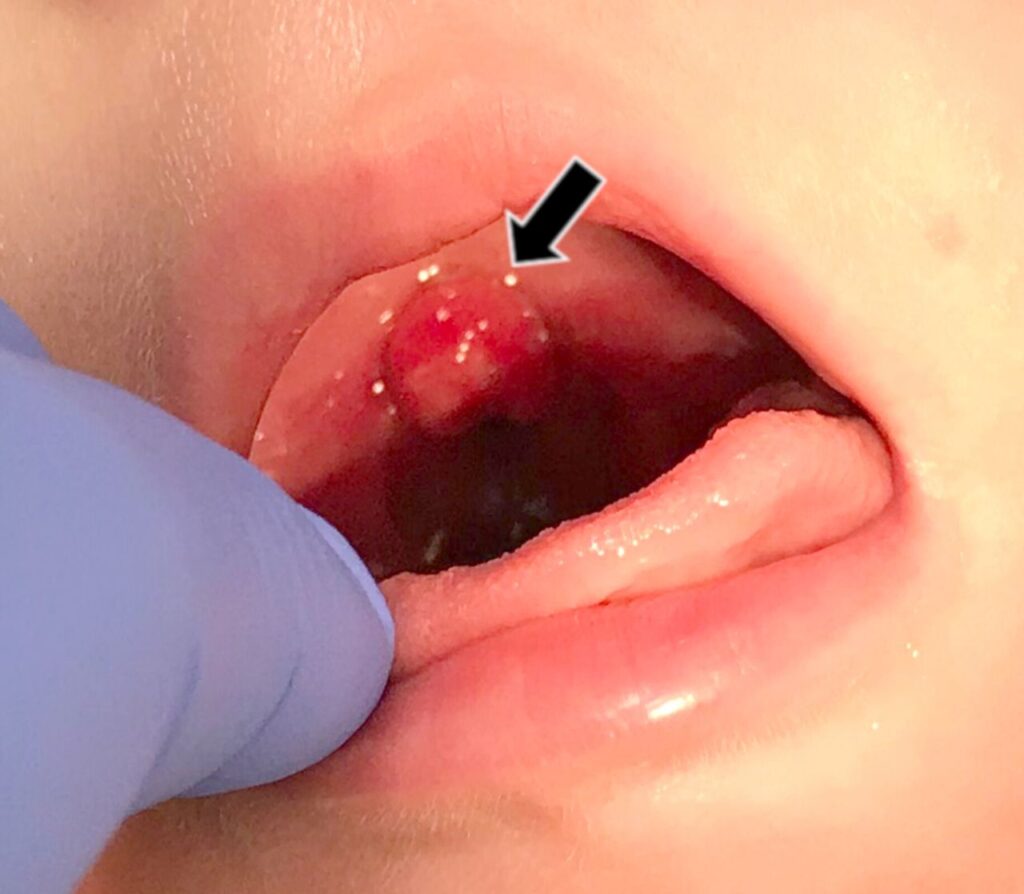
Clinical Presentation: Symptoms of Pharyngitis Caused by H. parainfluenzae
Patients may present with signs and symptoms commonly seen in other types of bacterial pharyngitis:
- Sore throat and dysphagia
- Redness and swelling of the pharyngeal wall
- Low to moderate-grade fever
- Cervical lymphadenopathy
- Tonsillar exudates (occasionally)
- Malaise and headache
- Possible hoarseness or cough in co-infections
In children, symptoms can be more pronounced, with irritability, refusal to eat, and nasal congestion.
Differential Diagnosis: Distinguishing H. parainfluenzae from Other Causes
Due to overlapping features with viral and streptococcal pharyngitis, laboratory diagnostics are critical for accurate identification.
| Condition | Key Differentiators |
|---|---|
| Viral pharyngitis | Cough, conjunctivitis, rhinorrhea |
| Streptococcal pharyngitis | Sudden onset, absence of cough, petechiae on palate |
| H. parainfluenzae pharyngitis | Subacute course, mild exudate, history of immunosuppression |
Diagnostic Approach
1. Throat Swab and Culture
- Primary tool for identifying H. parainfluenzae
- Requires chocolate agar or enriched media for growth
- Incubation under CO₂-enhanced conditions improves yield
2. Polymerase Chain Reaction (PCR)
- Offers rapid and specific detection
- Useful in mixed or polymicrobial infections
3. Blood Cultures
- Consider in systemic symptoms or immunocompromised hosts
4. Antibiotic Sensitivity Testing
- Essential due to rising resistance among Haemophilus species
- Beta-lactamase production is a concern in some strains
Treatment Strategies for H. parainfluenzae-Induced Pharyngitis
Prompt initiation of appropriate antibiotic therapy leads to rapid symptom resolution and prevents complications.
First-Line Antibiotics
- Amoxicillin-clavulanate: Preferred due to beta-lactamase activity
- Cefuroxime or Cefdinir: Effective cephalosporin options
Alternatives
- Azithromycin or Clarithromycin: For penicillin-allergic individuals
- Levofloxacin: Reserved for resistant cases or adults with severe disease
Supportive Therapy
- Analgesics (paracetamol, ibuprofen)
- Warm saline gargles
- Adequate hydration and vocal rest
- Use of humidifiers in dry environments
Complications from Untreated or Inadequately Treated Infections
Failure to treat pharyngitis due to H. parainfluenzae can lead to complications, particularly in at-risk populations.
- Peritonsillar abscess
- Otitis media
- Sinusitis
- Bronchitis or pneumonia
- Bacteremia (especially in immunocompromised hosts)
Prevention and Infection Control
While complete prevention is not always feasible, several measures can reduce incidence:
- Avoiding close contact with individuals displaying respiratory symptoms
- Proper hand hygiene
- Smoking cessation
- Judicious use of corticosteroids and immunosuppressants
- Monitoring and treating chronic upper respiratory tract issues
Haemophilus parainfluenzae in Clinical Context
Although often overshadowed by more common pathogens, H. parainfluenzae deserves attention due to its emerging role in opportunistic respiratory infections. Its increasing recognition as a causative agent in pharyngitis highlights the need for tailored diagnostic protocols and specific antimicrobial therapy.
Frequently Asked Questions
Is pharyngitis due to Haemophilus parainfluenzae contagious?
Yes. It may spread through respiratory droplets, especially in close-contact environments.
Can this infection resolve without antibiotics?
In immunocompetent individuals, mild infections might resolve, but antibiotic therapy is usually recommended to prevent progression or complications.
How is it different from strep throat?
Unlike Streptococcus pyogenes, H. parainfluenzae requires specific culture conditions and may not present with a high fever or petechiae.
Is it common in children?
It is less common than viral or streptococcal infections in children, but can occur, particularly in those with underlying conditions.
Can reinfection occur?
Yes. Recurrent infections are possible in individuals with persistent risk factors or compromised immunity.
Pharyngitis caused by Haemophilus parainfluenzae represents a clinically significant but often underdiagnosed condition. Accurate identification via culture or molecular testing, combined with targeted antibiotic therapy, ensures effective management. Raising clinical awareness of this pathogen is essential in both primary and specialized care settings to minimize complications and enhance patient outcomes.