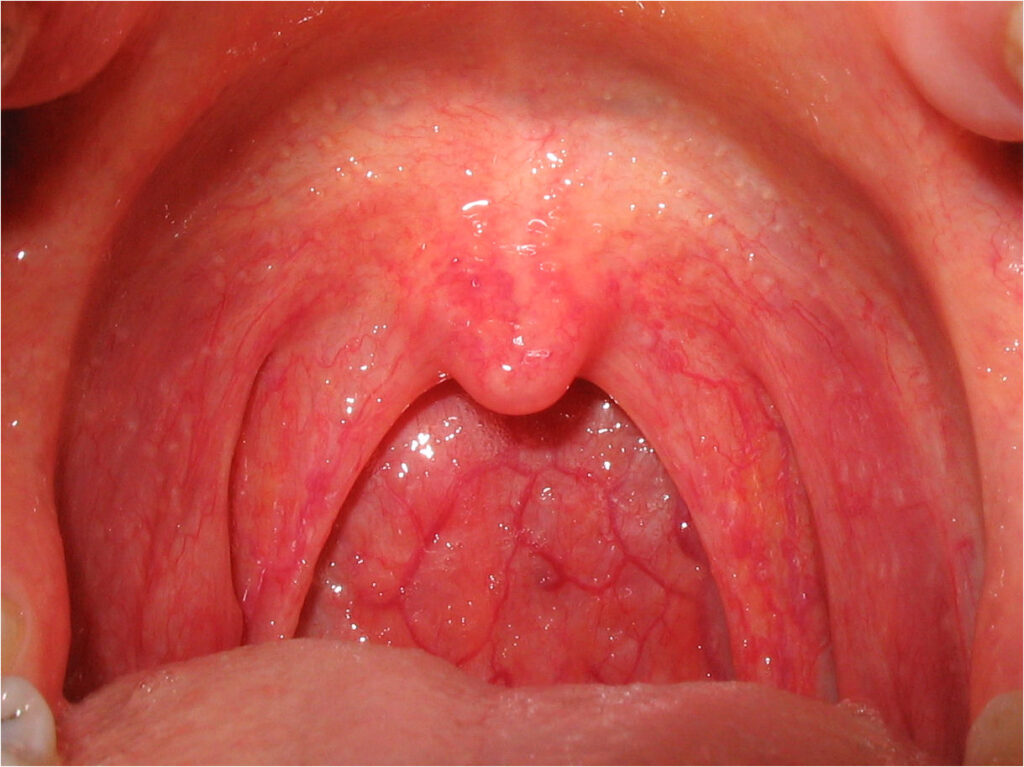
it is commonly referred to as a sore throat, is the inflammation of the pharynx — the anatomical region situated at the back of the throat. This condition, often triggered by viral or bacterial infections, affects individuals across all age groups. Pharyngitis may be acute or chronic, and understanding its underlying cause is vital for effective treatment and prevention.
Understandin and Its Classifications
Pharyngitis is categorized based on its duration and cause:
1. Acute Pharyngitis
- Onset: Sudden, short duration (up to 2 weeks)
- Most cases are viral in origin (e.g., rhinovirus, adenovirus)
- Bacterial causes include Streptococcus pyogenes (Group A Streptococcus)
2. Chronic Pharyngitis
- Duration: More than 3 weeks
- Associated with irritants such as smoke, pollution, allergies, or chronic sinusitis
Causes: Viral, Bacterial, and Other Triggers
Viral Causes (70–90% of Acute Cases)
- Rhinovirus
- Coronavirus
- Influenza and Parainfluenza viruses
- Epstein–Barr virus (mononucleosis)
- Herpes simplex virus
Bacterial Causes
- Group A Streptococcus (most common)
- Corynebacterium diphtheriae
- Mycoplasma pneumoniae
- Chlamydia pneumoniae
Non-Infectious Causes
- Allergens (pollen, dust)
- Smoking or second-hand smoke
- Dry air
- Gastroesophageal reflux disease (GERD)
- Prolonged voice strain
Recognizing the Symptoms of Pharyngitis
The presentation may vary depending on the underlying etiology:
Common Symptoms
- Throat pain or scratchiness
- Difficulty swallowing
- Swollen, red pharyngeal tissues
- Fever
- Fatigue
- Swollen lymph nodes in the neck
Viral Pharyngitis Symptoms
- Runny nose
- Hoarseness
- Conjunctivitis
- Cough
Bacterial Pharyngitis Symptoms
- Sudden sore throat onset
- High-grade fever
- Headache
- Abdominal pain (especially in children)
- Absence of cough
Complications of Untreated
When left untreated — especially bacterial pharyngitis — complications can occur:
- Peritonsillar abscess
- Acute rheumatic fever
- Post-streptococcal glomerulonephritis
- Otitis media
- Sinusitis
Diagnostic Approach
A structured diagnostic process aids in differentiating bacterial from viral causes and prevents unnecessary antibiotic use.
1. Clinical Scoring: Centor Criteria
Used to evaluate the probability of Group A Streptococcal infection.
| Criteria | Points |
|---|---|
| Fever | 1 |
| Tonsillar exudates | 1 |
| Tender anterior cervical nodes | 1 |
| Absence of cough | 1 |
| Age 3–14 | 1 |
| Age 15–44 | 0 |
| Age ≥45 | -1 |
Score ≥3 suggests bacterial etiology and supports further testing or empirical antibiotics.
2. Rapid Antigen Detection Test (RADT)
- Provides results within minutes
- High specificity for Group A Streptococcus
3. Throat Culture
- Gold standard
- More sensitive than RADT but slower (24–48 hours)
4. Monospot Test
- Used for suspected Epstein–Barr virus (mononucleosis)
Treatment Options
Viral Pharyngitis
No specific antiviral treatment is required. Supportive care includes:
- Warm saline gargles
- Analgesics (acetaminophen or ibuprofen)
- Adequate hydration
- Throat lozenges
Bacterial Pharyngitis (Streptococcal)
Early antibiotic therapy is crucial to reduce symptoms, transmission, and complications.
First-line Antibiotics:
- Penicillin V (10-day course)
- Amoxicillin (commonly used in pediatric cases)
Alternatives for Penicillin Allergy:
- Cephalexin
- Clindamycin
- Azithromycin
Home Care and Lifestyle Modifications
Supportive measures help ease discomfort and accelerate recovery:
- Use a humidifier in dry environments
- Avoid smoking and exposure to pollutants
- Consume warm broths and teas
- Rest and limit vocal strain
Prevention
General Preventive Strategies
- Frequent handwashing
- Avoiding contact with infected individuals
- Covering mouth and nose while sneezing or coughing
Vaccination
- Influenza vaccination reduces the incidence of flu-related pharyngitis
- COVID-19 vaccine to prevent viral pharyngitis associated with SARS-CoV-2
Pharyngitis in Children vs. Adults
Children are more susceptible to bacterial pharyngitis, particularly Group A Streptococcal infections. Adults tend to experience viral pharyngitis more frequently. Recognizing these age-based patterns assists clinicians in accurate diagnosis and management.
Frequently Asked Questions
What is the most common cause of pharyngitis?
Viruses are the leading cause, especially rhinovirus and influenza.
When should I see a doctor for a sore throat?
Seek medical attention if the sore throat is severe, lasts more than a week, or is accompanied by high fever, rash, or difficulty breathing.
Can pharyngitis be prevented?
Yes. Good hygiene, avoiding sick contacts, and staying updated on vaccines significantly reduce the risk.
Are antibiotics always needed for pharyngitis?
No. Antibiotics are only effective for bacterial causes and unnecessary use contributes to resistance.
Is pharyngitis contagious?
Yes. Most forms, especially viral and bacterial, can be transmitted via respiratory droplets.
Pharyngitis, though often benign, requires careful assessment to distinguish between viral and bacterial origins. Prompt and appropriate management not only relieves symptoms but also prevents complications and community spread. As healthcare providers, we must continue to emphasize evidence-based treatment, reduce antibiotic misuse, and educate the public on prevention and early intervention.