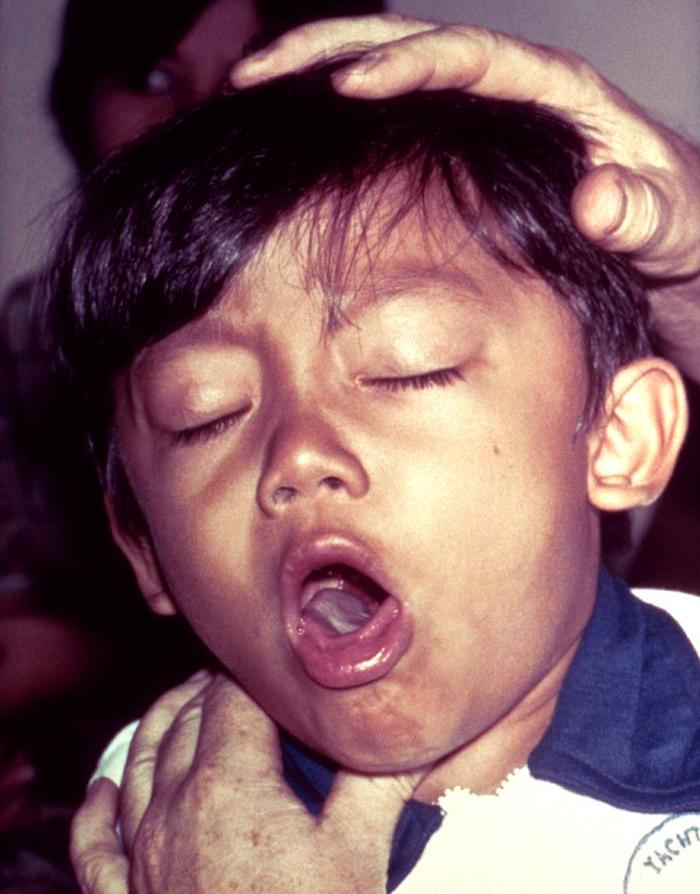
it is commonly known as whooping cough, is a highly contagious respiratory infection caused by Bordetella pertussis. This bacterial illness is characterized by severe coughing fits followed by a high-pitched “whoop” sound during inhalation. While it can affect individuals of all ages, infants under one year are at the highest risk of complications and mortality. The disease is preventable with timely vaccination and manageable with early diagnosis and treatment.
Etiology and Transmission
Causative Agent
Pertussis is caused by the Gram-negative coccobacillus Bordetella pertussis, which adheres to the cilia of the respiratory epithelium and releases toxins that damage tissue and interfere with the immune response.
Mode of Transmission
Pertussis is transmitted via airborne droplets when an infected person coughs, sneezes, or talks. It is highly contagious, with an attack rate exceeding 80% among susceptible household contacts.
Clinical Stages of Infection
it progresses through three distinct stages, each with characteristic clinical features:
1. Catarrhal Stage (1–2 weeks)
- Mild coughing
- Nasal congestion and rhinorrhea
- Low-grade fever
- Often mistaken for the common cold
- Most infectious phase
2. Paroxysmal Stage (2–6 weeks)
- Intense, repetitive coughing fits (paroxysms)
- Post-tussive vomiting
- Inspiratory “whoop” (less common in vaccinated individuals and infants)
- Apnea and cyanosis in infants
3. Convalescent Stage (2–3 weeks or longer)
- Gradual recovery
- Coughing becomes less severe
- Susceptibility to secondary respiratory infections remains high
in Infants: A Critical Risk Group
Infants under six months often present atypically, lacking the characteristic “whoop.” Instead, they may experience:
- Gasping
- Apnea
- Cyanotic spells
- Seizures (in severe cases)
- Life-threatening pneumonia
Infants represent the majority of pertussis-related hospitalizations and deaths due to immature immune systems and incomplete vaccination schedules.
Diagnosis
Early and accurate diagnosis is essential, especially in infants. Diagnostic methods include:
1. Polymerase Chain Reaction (PCR)
- Detects B. pertussis DNA in nasopharyngeal swabs
- High sensitivity and rapid turnaround
2. Culture
- Gold standard but less sensitive
- Requires specialized media (Bordet–Gengou or Regan–Lowe)
3. Serology
- Measures antibodies, useful in later stages
4. CBC with Differential
- Elevated lymphocyte count (lymphocytosis) is a hallmark in young children
Management and Treatment
1. Antibiotic Therapy
- Macrolides (azithromycin, erythromycin, clarithromycin) are first-line
- Reduces transmission if administered early
- Little effect on symptoms once paroxysmal stage begins
2. Supportive Care
- Oxygen therapy for severe hypoxemia
- Suctioning of mucus in infants
- Hydration and nutritional support
- Mechanical ventilation in cases of respiratory failure
3. Hospitalization
- Required for infants under six months or those with apnea, cyanosis, or complications
Vaccination: Prevention is Paramount
Vaccination remains the most effective tool in controlling pertussis transmission.
1. DTaP (Diphtheria, Tetanus, acellular Pertussis)
- Administered to infants and children at 2, 4, 6, and 15–18 months, and again at 4–6 years
2. Tdap (Tetanus, Diphtheria, acellular Pertussis)
- Booster for adolescents at 11–12 years
- Recommended for pregnant women during each pregnancy (preferably at 27–36 weeks gestation)
- Given to adults in place of one Td booster
3. Cocooning Strategy
- Vaccinating all close contacts of newborns to form a protective “cocoon”
Complications
Without treatment or timely intervention, pertussis can lead to serious complications, especially in infants:
- Pneumonia
- Seizures
- Encephalopathy
- Rib fractures (from severe coughing)
- Apnea
- Death
Epidemiology and Resurgence of cough and Pertussis
Global Trends
Despite high vaccine coverage, pertussis cases have resurged in recent decades. Contributing factors include:
- Waning immunity post-vaccination
- Decreased natural boosting due to lower exposure
- Evolution of B. pertussis strains
- Underdiagnosis and underreporting
Outbreak Settings
- Schools and childcare centers
- Healthcare environments
- Communities with low vaccination rates
Public Health Measures and Surveillance
Effective public health strategies are essential for pertussis control:
- Prompt case notification
- Post-exposure prophylaxis for contacts
- Immunization campaigns
- Health education on vaccination importance
Frequently Asked Questions:
What is pertussis?
Pertussis, or whooping cough, is a contagious respiratory disease caused by Bordetella pertussis, marked by severe coughing spells.
How is pertussis treated?
Early antibiotic therapy with macrolides is effective. Supportive care is crucial for infants and those with severe symptoms.
Can adults get pertussis?
Yes. Immunity wanes over time, making adolescents and adults susceptible without booster vaccines like Tdap.
Is pertussis dangerous for babies?
Yes. Infants are at the highest risk for complications such as apnea, pneumonia, and death. Vaccination and early detection are key.
How effective is the pertussis vaccine?
DTaP and Tdap vaccines offer strong protection, but immunity decreases over time, requiring boosters and maternal immunization for infants’ protection.
Pertussis remains a public health concern despite widespread immunization. Understanding its clinical stages, ensuring early diagnosis, and promoting complete vaccination schedules are essential steps to preventing severe disease and community outbreaks. Coordinated public health action and awareness are critical in safeguarding vulnerable populations, especially infants, against this preventable but potentially life-threatening disease.