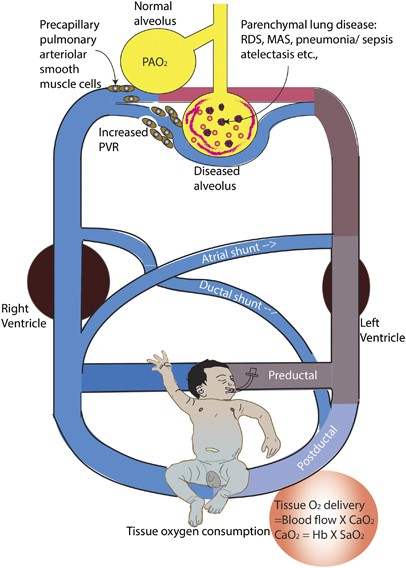
Persistent pulmonary hypertension of the newborn (PPHN) is a critical condition characterized by the failure of the normal circulatory transition that occurs after birth. It results in sustained elevated pulmonary vascular resistance (PVR), leading to right-to-left shunting of blood and severe hypoxemia. Immediate diagnosis and intervention are essential to reduce mortality and long-term morbidity.
Understanding Fetal and Neonatal Circulatory Transition
In utero, the fetal circulation bypasses the lungs through the ductus arteriosus and foramen ovale. At birth, the lungs expand, pulmonary vessels dilate, and systemic circulation assumes dominance.
In PPHN, this transition fails, maintaining high PVR and right-to-left shunting through fetal channels, thus limiting oxygen exchange and causing hypoxemia.
Causes and Risk Factors of PPHN in Neonates
1. Underlying Conditions Leading to PPHN
- Meconium Aspiration Syndrome (MAS)
- Neonatal Pneumonia
- Respiratory Distress Syndrome (RDS)
- Sepsis
- Birth asphyxia
- Pulmonary hypoplasia (e.g., congenital diaphragmatic hernia)
2. Idiopathic PPHN
- Diagnosed when no clear precipitating condition is found.
- May involve abnormal muscularization of pulmonary arterioles.
3. Maternal and Perinatal Risk Factors
- Diabetes mellitus
- Cesarean section without labor
- Use of nonsteroidal anti-inflammatory drugs (NSAIDs) during late pregnancy
- Perinatal hypoxia or acidosis
Clinical Manifestations of Persistent Pulmonary Hypertension of the Newborn
1. Signs and Symptoms
- Cyanosis unresponsive to oxygen
- Tachypnea and respiratory distress
- Labile oxygen saturation levels
- Low systemic blood pressure
- Heart murmur (due to tricuspid regurgitation)
2. Oxygen Saturation Gradient
- 10% difference between pre-ductal (right hand) and post-ductal (lower extremities) saturations
Pathophysiology of PPHN
This sequence highlights the central mechanism of PPHN, where elevated PVR leads to shunting and systemic hypoxia despite adequate oxygen delivery.
Diagnostic Evaluation of PPHN
1. Echocardiography
- Confirms elevated pulmonary pressures
- Identifies right-to-left shunting and excludes structural congenital heart defects
2. Pre- and Post-Ductal Pulse Oximetry
- Assesses oxygen saturation differential
- Non-invasive screening tool
3. Chest Radiograph
- Evaluates underlying lung pathology such as MAS or pneumonia
4. Blood Gases
- Shows respiratory and metabolic acidosis
- Hypoxemia refractory to conventional oxygen therapy
5. Laboratory Investigations
- Blood cultures, complete blood count, and C-reactive protein for infection
- Coagulation profile if disseminated intravascular coagulation is suspected
Management Strategies for PPHN
1. Supportive Respiratory Management
- Mechanical Ventilation: Maintains adequate oxygenation and prevents acidosis
- High-Frequency Oscillatory Ventilation (HFOV): Used in severe cases
- Surfactant Therapy: Beneficial in cases with underlying RDS or MAS
2. Pulmonary Vasodilation
- Inhaled Nitric Oxide (iNO):
- Selectively dilates pulmonary vasculature
- Reduces the need for extracorporeal membrane oxygenation (ECMO)
- Sildenafil or Milrinone:
- Used as adjuncts or alternatives to iNO
3. Extracorporeal Membrane Oxygenation (ECMO)
- Life-saving intervention for severe, unresponsive PPHN
- Temporarily supports gas exchange while allowing pulmonary vasculature to recover
4. Cardiovascular Support
- Inotropes (e.g., dopamine, dobutamine) to maintain systemic blood pressure and perfusion
5. Thermal and Metabolic Stability
- Maintain normothermia
- Correct metabolic acidosis, hypoglycemia, and electrolyte imbalances
Prognosis and Long-Term Outcomes
1. Survival Rates
- Advances in neonatal care have significantly improved survival
- Mortality remains high in cases requiring ECMO
2. Neurodevelopmental Outcomes
- Risk of hearing impairment, cognitive delays, or motor deficits
- Requires follow-up and early intervention programs
3. Pulmonary Sequelae
- Most infants recover pulmonary function
- Some may have persistent pulmonary hypertension or reactive airway disease
Prevention and Risk Mitigation
- Proper prenatal care and avoidance of late-term NSAID use
- Anticipation of risk in high-risk pregnancies (e.g., diabetic mothers, cesarean delivery)
- Immediate neonatal resuscitation and monitoring in perinatal hypoxia
Frequently Asked Questions:
What is the main cause of persistent pulmonary hypertension in newborns?
The most common causes include meconium aspiration syndrome, pneumonia, and birth asphyxia leading to failure in postnatal pulmonary vascular adaptation.
How is PPHN diagnosed?
Diagnosis relies on clinical signs, echocardiography, and pre- and post-ductal oxygen saturation differences, along with ruling out structural heart defects.
Can PPHN resolve completely?
Yes, with timely intervention, many infants recover fully. However, long-term follow-up is necessary to monitor neurodevelopmental and pulmonary outcomes.
Is PPHN preventable?
Not entirely, but appropriate maternal care, monitoring high-risk pregnancies, and careful delivery management can significantly reduce the risk.
When is ECMO used in PPHN?
ECMO is used in cases of severe, refractory hypoxemia that do not respond to conventional therapies, including iNO and ventilatory support.
Persistent pulmonary hypertension of the newborn is a life-threatening condition requiring prompt diagnosis and comprehensive treatment. Through targeted respiratory support, pulmonary vasodilation, and advanced interventions such as ECMO, survival and long-term outcomes have greatly improved. Early recognition and continuous monitoring are essential for optimizing neonatal health and preventing long-term complications.