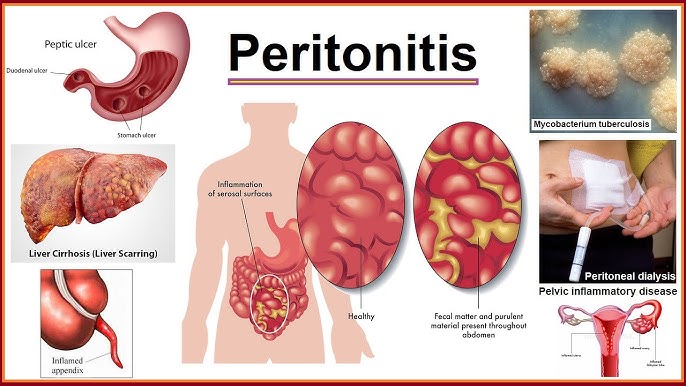
Peritonitis is a severe and potentially life-threatening inflammation of the peritoneum—the thin layer of tissue lining the inside of the abdominal wall and covering the abdominal organs. This condition demands urgent medical attention, as delayed treatment can result in systemic infection, organ failure, or death.
Understanding Peritonitis: Definition and Clinical Overview
Peritonitis occurs when the peritoneal lining becomes inflamed, usually due to bacterial or fungal infections. It may result from a breach in the gastrointestinal tract, such as a perforated ulcer, ruptured appendix, or bowel obstruction. The condition can be classified as primary, secondary, or tertiary peritonitis, based on origin and severity.
Common Causes of Peritonitis
Understanding the etiology is critical for appropriate treatment. Key causes include:
1. Primary (Spontaneous Bacterial Peritonitis – SBP)
- Common in patients with liver cirrhosis and ascites
- Caused by translocation of gut bacteria
2. Secondary Peritonitis
- Due to a rupture or perforation in abdominal organs
- Common causes:
- Appendicitis
- Perforated peptic ulcer
- Diverticulitis
- Pancreatitis with necrosis
- Surgical complications
- Trauma to abdominal wall or viscera
3. Tertiary Peritonitis
- Persistent or recurrent infection following treatment of primary or secondary peritonitis
- Frequently seen in immunocompromised patients
Signs and Symptoms of Peritonitis
Clinical presentation can vary based on the underlying cause and severity. Common symptoms include:
- Severe abdominal pain or tenderness
- Rigid or distended abdomen
- Fever and chills
- Nausea and vomiting
- Loss of appetite
- Fatigue and malaise
- Rapid heartbeat and low blood pressure
- Reduced urine output
- Altered mental status, especially in elderly or septic patients
Diagnostic Evaluation of Peritonitis
Prompt diagnosis is essential for patient survival. Diagnostic approaches include:
1. Physical Examination
- Guarding, rebound tenderness, and reduced bowel sounds
2. Laboratory Investigations
- Complete blood count (CBC): Elevated white blood cells
- Blood cultures: Identify systemic infection
- Electrolytes and renal function tests
- Liver function tests in cirrhotic patients
3. Peritoneal Fluid Analysis (Paracentesis)
- Diagnostic in ascitic patients
- Cell count, culture, and gram stain of ascitic fluid
4. Imaging Studies
- Abdominal X-rays: Identify free air under diaphragm (perforation)
- Ultrasound: Detect ascitic fluid or abscess
- CT scan: Visualize abdominal organs and complications
Treatment Strategies for Peritonitis
The management of peritonitis depends on its type and cause. Immediate hospitalization is typically required.
1. Antibiotic Therapy
- Empirical broad-spectrum antibiotics targeting gram-positive, gram-negative, and anaerobic bacteria
- Adjusted after culture results
- Antifungals for suspected fungal peritonitis
2. Surgical Intervention
- Required for secondary peritonitis due to perforation, abscess, or necrosis
- Procedures include:
- Appendectomy
- Resection of perforated bowel
- Abscess drainage
- Peritoneal lavage
3. Supportive Care
- Intravenous fluids for hydration
- Electrolyte balance
- Vasopressors for septic shock
- Nutritional support
Complications Associated with Peritonitis
If untreated or inadequately managed, peritonitis can lead to:
- Sepsis and septic shock
- Multiple organ dysfunction syndrome (MODS)
- Intra-abdominal abscesses
- Adhesions and bowel obstruction
- Acute kidney injury
- Mortality, especially in elderly or immunocompromised patients
Prevention of Peritonitis
Preventive strategies can significantly reduce the incidence, particularly in high-risk individuals.
- Proper peritoneal dialysis hygiene in dialysis patients
- Timely treatment of abdominal infections
- Avoiding non-sterile invasive procedures
- Regular monitoring in cirrhotic patients with ascites
Frequently Asked Questions:
What is the main cause of peritonitis?
Peritonitis is most commonly caused by bacterial infection due to a rupture in an abdominal organ, such as in appendicitis or perforated ulcers.
How is peritonitis diagnosed?
Through physical exam, blood tests, imaging, and peritoneal fluid analysis. In patients with ascites, diagnostic paracentesis is essential.
Can peritonitis be cured?
Yes, with prompt antibiotic therapy and surgical treatment if needed. Delay in treatment increases risk of complications.
Is peritonitis contagious?
No, peritonitis is not contagious. It is an internal condition and does not spread through contact.
Who is most at risk of developing peritonitis?
Patients with liver cirrhosis, those undergoing peritoneal dialysis, individuals with compromised immune systems, and people with intra-abdominal infections.
Peritonitis is a medical emergency requiring swift identification and intervention. By understanding its types, causes, and clinical presentation, healthcare providers can deliver timely, life-saving care. Preventive measures and vigilant monitoring in high-risk populations play a pivotal role in reducing morbidity and mortality associated with this critical condition.