Peripheral T-cell lymphoma (PTCL) refers to a diverse group of rare and aggressive non-Hodgkin lymphomas (NHL) derived from mature T-lymphocytes. Unlike B-cell lymphomas, PTCLs exhibit complex clinical behaviors and are frequently associated with poor prognosis due to late-stage detection and limited response to conventional therapies.
Accounting for approximately 10–15% of all NHLs in Western populations, PTCL encompasses multiple subtypes with distinct pathological, genetic, and clinical profiles, often requiring individualized treatment approaches.
Classification of PTCL Subtypes
The World Health Organization (WHO) classifies PTCL into several categories based on histology, immunophenotype, and molecular markers.
Major PTCL Subtypes:
| Subtype | Key Characteristics |
|---|---|
| PTCL, Not Otherwise Specified (NOS) | Most common, heterogeneous morphology |
| Angioimmunoblastic T-cell lymphoma (AITL) | Immune dysfunction, systemic symptoms |
| Anaplastic large cell lymphoma (ALCL) | ALK+ or ALK– variants, large anaplastic cells |
| Extranodal NK/T-cell lymphoma, nasal type | Associated with Epstein-Barr virus (EBV) |
| Enteropathy-associated T-cell lymphoma (EATL) | Linked to celiac disease, intestinal involvement |
| Hepatosplenic T-cell lymphoma (HSTCL) | Occurs in immunocompromised patients |
These subtypes exhibit different clinical manifestations, prognosis, and treatment responses, emphasizing the importance of precise diagnosis.
Pathophysiology and Molecular Features
Peripheral T-cell lymphomas originate from mature post-thymic T-cells that undergo malignant transformation due to genetic and epigenetic alterations.
Common Molecular Abnormalities:
- TCR gene rearrangements confirming T-cell lineage
- CD30 expression in ALCL and some PTCL-NOS cases
- Mutations in genes like RHOA, TET2, IDH2, DNMT3A (especially in AITL)
- ALK gene translocation in ALK-positive ALCL
The tumor microenvironment, including inflammatory and immune cells, plays a pivotal role in disease progression, particularly in AITL, which presents with immune dysregulation and autoimmune-like features.
Clinical Presentation and Symptoms
Peripheral T-cell lymphoma symptoms are often non-specific and resemble other forms of aggressive lymphomas. Patients typically present with:
- Painless lymphadenopathy (enlarged lymph nodes)
- B-symptoms: fever, night sweats, weight loss
- Fatigue and generalized malaise
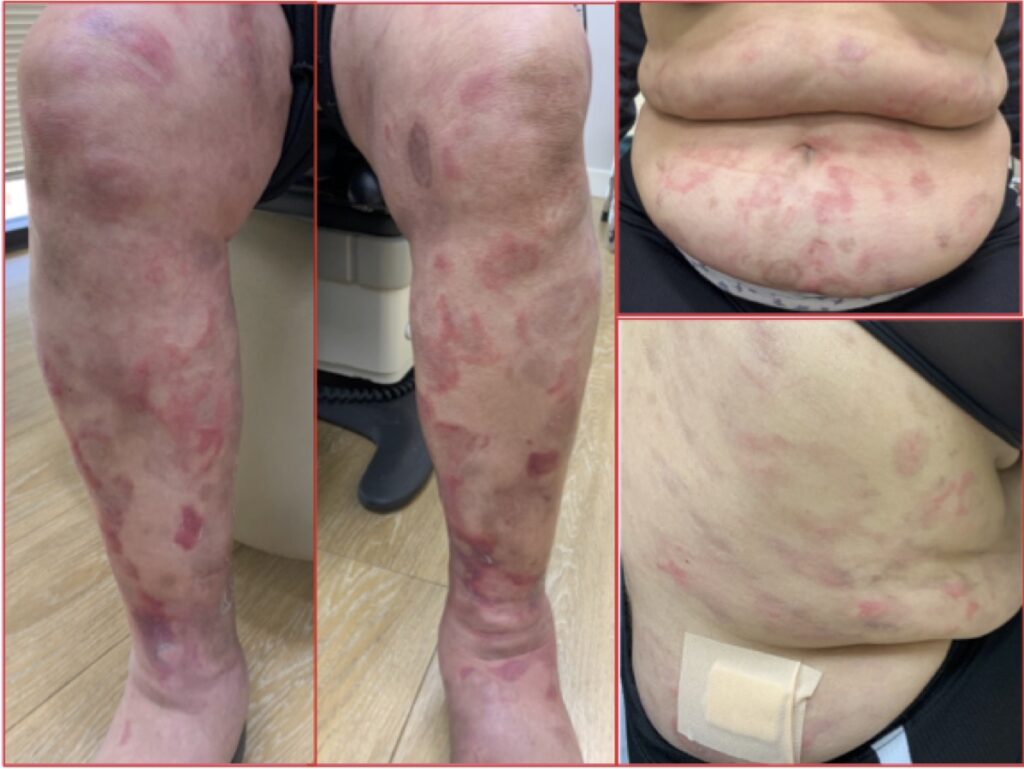
- Skin rashes or nodules (cutaneous involvement in some subtypes)
- Organomegaly: spleen or liver enlargement
- Gastrointestinal distress in enteropathy-associated variants
- Nasal obstruction or bleeding in NK/T-cell lymphoma
Due to their systemic nature and rapid progression, PTCLs are usually diagnosed at advanced stages (Stage III or IV).
Diagnostic Approach to PTCL
The diagnosis of peripheral T-cell lymphoma involves a combination of histopathological analysis, immunophenotyping, molecular studies, and imaging.
Key Diagnostic Tools:
- Histopathology: Reveals atypical T-cells, mitotic figures, necrosis
- Immunohistochemistry (IHC): CD3+, CD4+, CD8+, CD30, ALK, Ki-67
- Flow Cytometry: Confirms aberrant T-cell markers
- Molecular testing: TCR gene rearrangements, mutation panels
- Imaging (PET-CT): Determines disease extent and organ involvement
- Bone marrow biopsy: Evaluates marrow infiltration
Accurate subtype classification is essential to determine the appropriate treatment pathway and predict outcomes.
Staging and Prognostic Factors
The Ann Arbor staging system, typically used for lymphomas, also applies to PTCL:
- Stage I-II: Limited disease
- Stage III-IV: Advanced disease with multiple lymph node or extranodal involvement
Prognostic Indicators:
| Factor | Impact |
|---|---|
| Age >60 | Poorer prognosis |
| ECOG performance status ≥2 | Worse outcomes |
| Elevated LDH levels | Aggressive disease |
| Bone marrow involvement | Reduced survival |
| High Ki-67 index | Increased proliferation and relapse risk |
The International Prognostic Index (IPI) and Prognostic Index for PTCL (PIT) are widely used to stratify patients based on risk.
First-Line Treatment Strategies
Peripheral T-cell lymphomas are treated with multi-agent chemotherapy regimens, with or without stem cell transplantation.
Standard Regimen:
- CHOP (Cyclophosphamide, Doxorubicin, Vincristine, Prednisone): Common first-line therapy, though with limited efficacy in PTCL compared to B-cell lymphomas
Improved Regimens:
- CHOEP: CHOP plus etoposide (for younger patients with good performance status)
- Brentuximab vedotin + CHP: Approved for CD30+ PTCL, especially ALCL
Consolidation Therapy:
- Autologous stem cell transplant (ASCT): Recommended in first complete remission for eligible patients to improve progression-free survival
- Radiotherapy: May be added in localized disease
Management of Relapsed/Refractory PTCL
Relapse is common in PTCL, and prognosis after recurrence is generally poor. Salvage strategies include:
Approved Therapies:
- Brentuximab vedotin: For relapsed CD30+ PTCL
- Pralatrexate: Antifolate agent approved for relapsed PTCL
- Romidepsin and Belinostat: HDAC inhibitors used in second-line settings
- Duvelisib: PI3K-δ/γ inhibitor under investigation
Cellular Therapies and Transplantation:
- Allogeneic stem cell transplant: Potential curative option for chemosensitive relapsed PTCL
- CAR-T cell therapy: Under evaluation for T-cell malignancies
Response rates in relapsed settings are modest, necessitating participation in clinical trials where possible.
Emerging Therapies and Clinical Trials
Ongoing research is focused on molecularly targeted agents and immunotherapy strategies for PTCL:
- JAK/STAT inhibitors: Particularly in subtypes with pathway activation
- Checkpoint inhibitors: Limited efficacy so far, but under investigation
- CD47 and CD52 antibodies: Immune evasion blockers
- Bispecific T-cell engagers (BiTEs): New frontier for T-cell malignancies
- Epigenetic therapies: Targeting DNMT, TET2 mutations common in AITL
Precision oncology approaches using next-generation sequencing (NGS) to match therapies with mutational profiles hold promise for future management.
Prognosis and Survival Rates
Prognosis in peripheral T-cell lymphoma varies significantly by subtype and treatment response:
| PTCL Subtype | 5-Year Overall Survival |
|---|---|
| ALK+ ALCL | ~70–80% |
| ALK– ALCL | ~40–50% |
| PTCL-NOS | ~30–35% |
| AITL | ~30% |
| NK/T-cell lymphoma | ~40% (higher with early radiotherapy) |
The poor long-term outcomes in most PTCL subtypes highlight the urgency for improved diagnostic tools and therapeutic strategies.
Peripheral T-cell lymphoma represents a biologically and clinically heterogeneous group of aggressive lymphomas requiring meticulous diagnosis and individualized treatment strategies. While current therapies offer modest outcomes, emerging molecularly targeted and immunotherapeutic options signal hope for future advancements. Continued research, accurate subtyping, and early intervention are essential to improving survival in this challenging group of hematologic malignancies.