Bacteroides pelvic cellulitis is a severe bacterial infection that affects the pelvic region, often resulting from the proliferation of Bacteroides species, a group of anaerobic bacteria. These bacteria, while naturally occurring in the human gut and other mucosal surfaces, can become pathogenic under specific conditions, leading to inflammation, abscess formation, and tissue damage. This article explores the causes, symptoms, diagnostic methods, treatment options, and prevention strategies for Bacteroides pelvic cellulitis.
Causes and Risk Factors
Bacteroides species, particularly Bacteroides fragilis, are the primary culprits behind pelvic cellulitis. These anaerobes thrive in low-oxygen environments and can invade tissues when the natural barriers are compromised.
Common Causes:
- Surgical Procedures: Gynecological surgeries such as hysterectomies or cesarean sections can introduce Bacteroides to sterile pelvic regions.
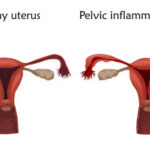
- Pelvic Inflammatory Disease (PID): A common precursor caused by ascending infections.
- Trauma: Physical injuries to the pelvic region can provide entry points for bacteria.
- Compromised Immunity: Conditions like diabetes or HIV can increase susceptibility.
Risk Factors:
- Recent pelvic or abdominal surgeries
- Intrauterine device (IUD) insertion
- Use of broad-spectrum antibiotics that disrupt normal flora
- Chronic inflammatory conditions
Symptoms of Bacteroides Pelvic Cellulitis
Recognizing symptoms early is crucial for effective treatment. Symptoms can range from mild to severe, depending on the extent of the infection.
Common Symptoms:
- Persistent pelvic pain
- Fever and chills
- Swelling and redness in the lower abdomen
- Foul-smelling vaginal discharge
- Fatigue and malaise
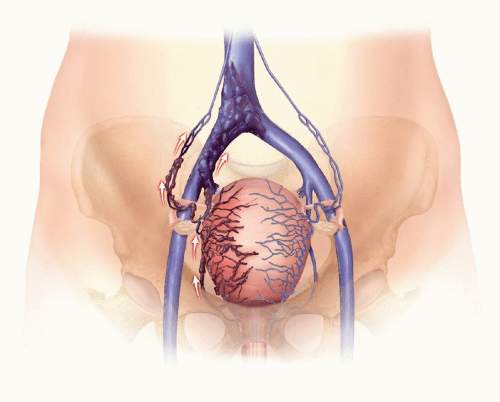
In advanced cases, abscess formation, sepsis, and systemic inflammation may occur, requiring immediate medical intervention.
Diagnosis
Timely and accurate diagnosis of Bacteroides pelvic cellulitis involves a combination of clinical evaluation, imaging, and microbiological testing.
Diagnostic Methods:
- Physical Examination: Identifies tenderness, swelling, and signs of systemic infection.
- Laboratory Tests: Complete blood count (CBC) may show elevated white blood cells; blood cultures may isolate Bacteroides species.
- Imaging: Ultrasound or CT scans help detect abscesses or tissue inflammation.
- Microbiological Cultures: Vaginal or pelvic fluid samples are analyzed to confirm the presence of Bacteroides.
Treatment Options
Treatment focuses on eradicating the infection, managing symptoms, and preventing complications.
Antibiotic Therapy:
The cornerstone of treatment is the administration of antibiotics effective against anaerobic bacteria. Commonly used antibiotics include:
- Metronidazole
- Clindamycin
- Carbapenems
Combination therapy may be required in severe cases to cover both anaerobic and aerobic pathogens.
Surgical Intervention:
- Abscess Drainage: Required for large or unresolving abscesses.
- Debridement: Removal of necrotic tissues to promote healing.
Supportive Care:
- Hydration and electrolyte balance
- Pain management
- Monitoring for signs of sepsis
Prevention Strategies
Preventing Bacteroides pelvic cellulitis involves addressing risk factors and maintaining good health practices.
Key Measures:
- Post-Surgical Care: Proper hygiene and follow-up reduce infection risk.
- Prompt Treatment of PID: Early management of infections can prevent complications.
- Judicious Antibiotic Use: Prevents disruption of natural flora.
- Safe Practices: Ensure sterile techniques during gynecological procedures.
Prognosis and Long-Term Outlook
With timely treatment, most patients recover fully from Bacteroides pelvic cellulitis. However, untreated or recurrent infections may lead to chronic pelvic pain, infertility, or systemic complications. Regular medical follow-ups and adherence to treatment protocols are essential for optimal recovery.