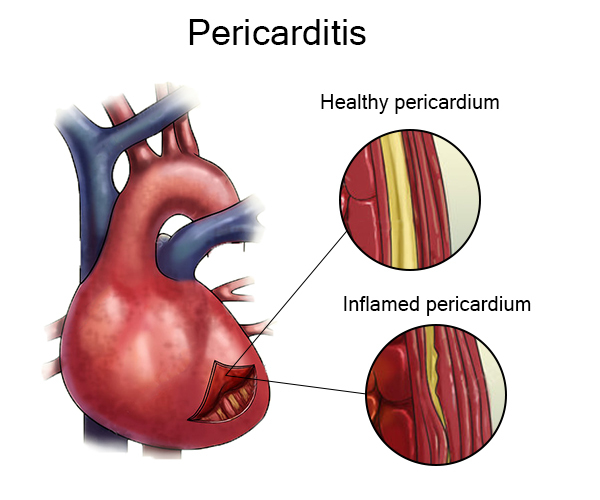
Pericarditis is an inflammatory condition affecting the pericardium, the thin, double-layered sac that surrounds and protects the heart. This inflammation can lead to chest pain, pericardial effusion, and, in severe cases, cardiac tamponade or constrictive pericarditis.
Types of Pericarditis and Their Classification
Pericarditis can be classified by duration and etiology.
Based on Duration
- Acute Pericarditis: Lasts less than 6 weeks; most common form.
- Subacute Pericarditis: Lasts from 6 weeks to 6 months.
- Chronic Pericarditis: Persists for more than 6 months.
- Recurrent Pericarditis: New episode after initial resolution.
Based on Cause
- Idiopathic (most common, presumed viral)
- Infectious (viral, bacterial, tuberculosis)
- Autoimmune (systemic lupus erythematosus, rheumatoid arthritis)
- Post-myocardial infarction (Dressler’s syndrome)
- Trauma or surgery-related
- Uremic
- Neoplastic
- Radiation-induced
Pathophysiology of Pericardial Inflammation
Inflammation of the pericardium leads to vascular permeability, exudation of protein-rich fluid, and leukocyte infiltration. In severe cases, this may result in fibrin deposition and adhesion between the pericardial layers.
Clinical Presentation: Recognizing the Symptoms of Pericarditis
Hallmark Features
- Chest Pain: Sharp and pleuritic, often relieved by sitting forward and worsened by lying down.
- Pericardial Friction Rub: A superficial, scratchy sound heard on auscultation.
- Fever: Mild in viral or idiopathic cases.
- Dyspnea: Especially with pericardial effusion.
Associated Symptoms
- Cough
- Fatigue
- Palpitations
- Light-headedness (if tamponade develops)
Diagnostic Approach to Pericarditis
Timely diagnosis relies on a combination of clinical, laboratory, and imaging findings.
Diagnostic Criteria (Requires at least two)
- Characteristic chest pain
- Pericardial friction rub
- ECG changes (widespread ST elevation and PR depression)
- New or worsening pericardial effusion
Electrocardiogram (ECG) Findings
- Stage I: Diffuse ST-segment elevation, PR segment depression
- Stage II: ST normalization
- Stage III: T wave inversion
- Stage IV: ECG returns to normal
Imaging and Tests
- Echocardiography: Assesses for pericardial effusion and cardiac function.
- Cardiac MRI/CT: Confirms inflammation and rules out constrictive pericarditis.
- Blood Tests:
- Elevated inflammatory markers (CRP, ESR)
- Leukocytosis
- Troponins may be slightly elevated
- Renal function and autoimmune panels if secondary cause suspected
Treatment Options for Pericarditis
First-Line Treatment (for idiopathic or viral causes)
- NSAIDs: Ibuprofen or aspirin to reduce inflammation and relieve pain.
- Colchicine: Reduces recurrence risk and shortens symptom duration.
- Activity Restriction: Avoid physical exertion for at least 1–3 months.
Adjunctive and Second-Line Therapies
- Corticosteroids: For patients unresponsive to NSAIDs or with autoimmune etiology; used cautiously due to higher recurrence risk.
- Immunosuppressive Agents: Azathioprine or anakinra in refractory or autoimmune cases.
- Antibiotics or Antitubercular therapy: If specific infection is identified.
Complications of Pericarditis
Pericardial Effusion
Fluid accumulation in the pericardial cavity that may progress to tamponade.
Cardiac Tamponade
Life-threatening condition with impaired cardiac filling; requires urgent pericardiocentesis.
Constrictive Pericarditis
Chronic scarring and loss of pericardial elasticity, leading to diastolic heart failure. Surgical pericardiectomy may be necessary.
Prognosis and Recurrence
Prognosis
Most cases of acute pericarditis resolve with appropriate therapy. Prognosis is favorable when underlying malignancy or infection is not present.
Risk of Recurrence
- Occurs in up to 30% of patients
- Higher risk in corticosteroid-treated or undertreated cases
Preventative strategy includes full treatment course with colchicine and avoidance of early physical activity.
Frequently Asked Questions
Q1. What triggers pericarditis most commonly?
Viral infections are the most common cause of acute pericarditis, followed by idiopathic and autoimmune disorders.
Q2. How is pericarditis pain different from heart attack pain?
Pericarditis pain is sharp and pleuritic, improves with leaning forward, while myocardial infarction pain is crushing and persistent.
Q3. Can pericarditis recur?
Yes, particularly if treatment is incomplete or if steroids are used prematurely. Colchicine reduces recurrence risk.
Q4. When is hospitalization required for pericarditis?
Hospitalization is advised in cases of fever >38°C, large pericardial effusion, immunosuppression, trauma, or suspected tamponade.
Q5. Is pericarditis fatal?
Rarely, but complications like tamponade or constrictive pericarditis can be fatal without prompt treatment.
Pericarditis is a common yet potentially serious cardiovascular condition. Early diagnosis, appropriate anti-inflammatory therapy, and close monitoring are essential to achieve full recovery and minimize complications. For recurrent or chronic cases, advanced management strategies and tailored treatment plans are critical to improving outcomes.