Pericardial malignant effusion refers to the accumulation of fluid in the pericardial sac surrounding the heart, due to cancerous involvement. This condition often signifies advanced malignancy and carries significant clinical implications. The fluid buildup can compress the heart, impair its function, and lead to life-threatening complications such as cardiac tamponade.
Pathophysiology of Malignant Pericardial Effusion
Malignant cells infiltrate the pericardium either directly or via lymphatic spread. This infiltration disrupts normal pericardial fluid homeostasis, resulting in excessive production or impaired drainage of pericardial fluid.
Common Cancers Causing Pericardial Effusion
- Lung carcinoma (most common)
- Breast cancer
- Lymphomas (Hodgkin and non-Hodgkin)
- Leukemia
- Melanoma
- Mesothelioma
These malignancies either metastasize to the pericardium or grow locally, triggering inflammation, angiogenesis, and increased vascular permeability.
Clinical Presentation and Symptoms
The symptomatology varies depending on the rate of fluid accumulation and volume. Rapid accumulation even in small amounts can cause tamponade, whereas slow accumulation might be asymptomatic until late stages.
Common Symptoms
- Dyspnea (shortness of breath)
- Chest pain or discomfort
- Orthopnea (difficulty breathing when lying down)
- Fatigue
- Tachycardia
- Hypotension
- Jugular venous distension
In severe cases, Beck’s triad—hypotension, muffled heart sounds, and elevated jugular venous pressure—indicates cardiac tamponade.
Diagnostic Evaluation
Prompt diagnosis is essential to prevent hemodynamic compromise.
Imaging Modalities
- Echocardiography: Gold standard for detecting pericardial effusion. Can assess effusion size, location, and cardiac tamponade signs.
- Chest CT and MRI: Used for detailed anatomical evaluation and to detect pericardial thickening, masses, or adjacent malignancies.
- Chest X-ray: May reveal cardiomegaly in large effusions but is less specific.
Pericardial Fluid Analysis
Performed via pericardiocentesis, fluid is aspirated for laboratory analysis:
- Cytology: Presence of malignant cells confirms diagnosis.
- Biochemical markers: Elevated LDH and protein content suggest exudative nature.
- Microbiological testing: Excludes infectious etiologies.
Additional Tests
- ECG: May show low QRS voltage or electrical alternans.
- Blood tests: Evaluate underlying malignancy and assess overall patient status.
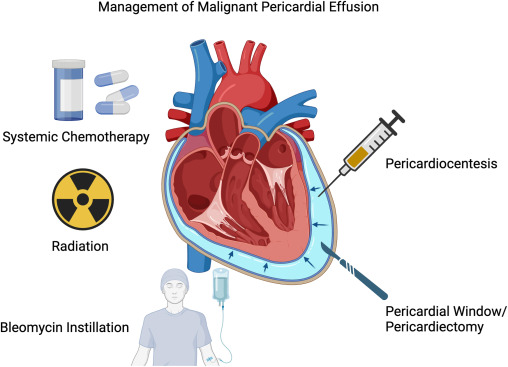
Treatment Approaches
Acute Management
Pericardiocentesis is the first-line treatment for symptomatic effusions or tamponade. It provides rapid relief and fluid for diagnostic evaluation.
Definitive Management
- Pericardial Window Surgery: A surgical opening is made in the pericardium to allow continuous drainage. Suitable for recurrent effusions.
- Indwelling Pericardial Catheters: For palliative care in patients with poor prognosis or repeated recurrence.
- Intrapericardial Chemotherapy: Agents like cisplatin or thiotepa may be instilled to reduce recurrence.
- Radiation Therapy: Targeted at tumor mass, particularly effective in lymphoma-related effusions.
Management of Underlying Malignancy
Oncological treatment—systemic chemotherapy, immunotherapy, or targeted therapy—can significantly reduce the recurrence of malignant effusions if the primary tumor responds well.
Prognosis and Outcomes
The prognosis of pericardial malignant effusion is closely tied to the stage and type of primary cancer. Overall, the condition is associated with a poor prognosis:
- Median survival after diagnosis: 3 to 6 months (varies with primary tumor)
- Better outcomes are noted in patients with chemotherapy-sensitive malignancies like lymphoma or leukemia.
Prognostic Indicators
- Presence of cardiac tamponade
- Rapid fluid reaccumulation
- Poor performance status
- Chemotherapy resistance
Pericardial malignant effusion is a serious oncologic complication requiring swift diagnosis and tailored intervention. Multimodal imaging, cytologic confirmation, and integrated oncologic management are vital. While palliative in most cases, timely intervention can significantly enhance quality of life and potentially extend survival in select cases.