Percutaneous coronary intervention (PCI) has revolutionized the management of coronary artery disease. However, despite advances in stent design and procedural techniques, thrombosis remains a serious complication, particularly in patients with high thrombus burden or acute coronary syndromes. Preventing thrombosis during and after PCI requires a comprehensive strategy involving pharmacologic and mechanical adjuncts tailored to individual risk profiles.
Mechanisms of Thrombus Formation During PCI
Thrombosis during PCI is initiated by endothelial disruption and exposure of subendothelial matrix proteins, triggering platelet activation and coagulation cascades. Shear stress, plaque rupture, and the presence of stents further exacerbate prothrombotic conditions.
Pharmacologic Adjuncts for Thrombosis Prevention in PCI
1. Dual Antiplatelet Therapy (DAPT)
DAPT remains the cornerstone of thrombosis prevention in PCI. The combination of aspirin and a P2Y12 receptor inhibitor significantly reduces the risk of stent thrombosis and recurrent ischemic events.
- Aspirin: Irreversibly inhibits thromboxane A2-mediated platelet aggregation.
- P2Y12 Inhibitors:
- Clopidogrel: Prodrug requiring hepatic activation, moderate potency
- Prasugrel: More potent, preferred in STEMI and high-risk PCI
- Ticagrelor: Reversible inhibitor with rapid onset, superior in ACS
Duration: Typically 6-12 months post-PCI, depending on stent type and bleeding risk.
2. Glycoprotein IIb/IIIa Inhibitors
These intravenous agents block the final common pathway of platelet aggregation by inhibiting fibrinogen binding.
- Agents: Abciximab, Eptifibatide, Tirofiban
- Use: Reserved for high thrombus burden, bailout situations, or STEMI with visible thrombus.
3. Anticoagulants
Intra-procedural anticoagulation minimizes acute thrombosis risk.
- Unfractionated Heparin (UFH): Standard anticoagulant during PCI
- Bivalirudin: Direct thrombin inhibitor; lowers bleeding risk; preferred in high-bleeding-risk patients
- Low Molecular Weight Heparin (LMWH): Used less commonly due to prolonged effect and limited reversibility
Mechanical and Device-Based Adjuncts in Thrombus Management
1. Thrombus Aspiration Devices
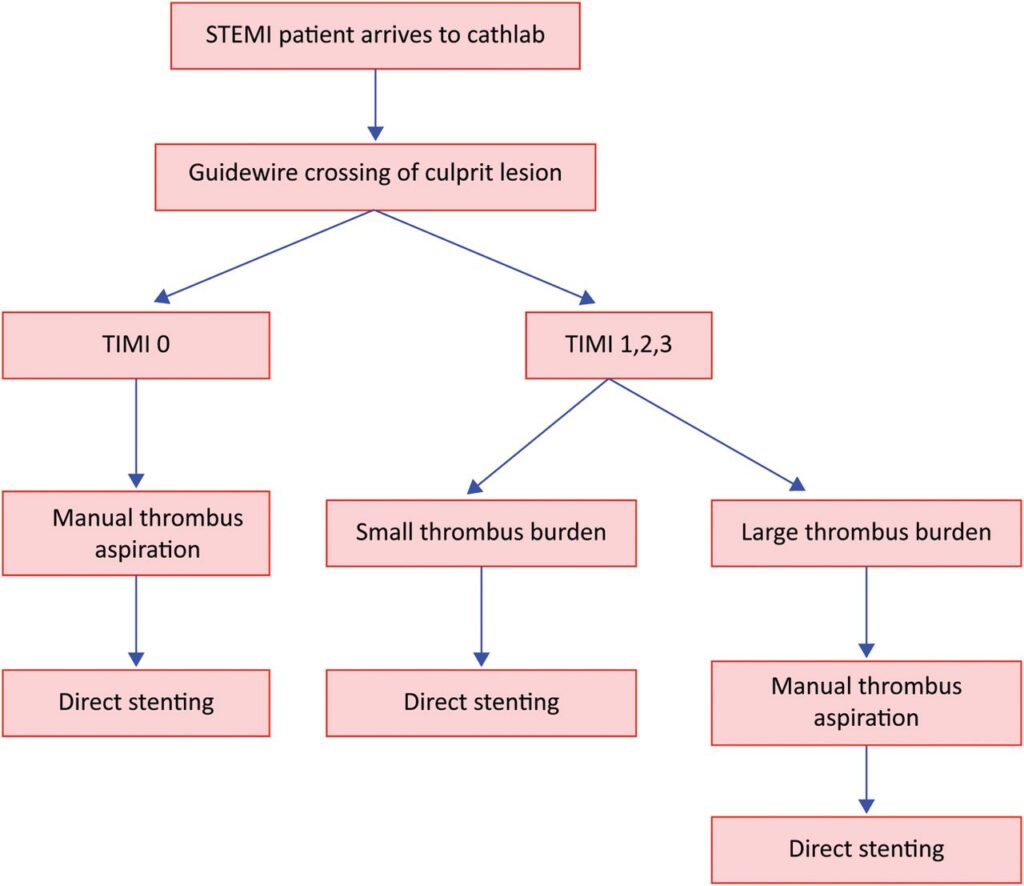
Mechanical removal of thrombus via aspiration catheters has been utilized in high-thrombus burden cases, especially in ST-elevation myocardial infarction (STEMI). Although large-scale trials (e.g., TASTE, TOTAL) showed no mortality benefit, selective use in high thrombus burden persists.
2. Distal Protection Devices
Primarily used in saphenous vein graft PCI to prevent distal embolization of thrombotic or atheromatous debris, minimizing no-reflow phenomenon.
3. Intravascular Imaging
While not an adjunct per se, tools like Optical Coherence Tomography (OCT) and Intravascular Ultrasound (IVUS) enhance lesion assessment, guide stent deployment, and identify thrombus morphology to tailor adjunctive therapy.
Novel and Emerging Antithrombotic Strategies
1. Cangrelor
An intravenous P2Y12 inhibitor with rapid onset and offset, ideal for bridging in patients not preloaded with oral antiplatelets.
- Indications: PCI in P2Y12-naïve patients, high thrombotic risk, or bridging to surgery
2. Factor Xa Inhibitors and DOACs in PCI
Although primarily used in atrial fibrillation and venous thromboembolism, studies are evaluating their potential in high-risk PCI patients, especially with concomitant atrial fibrillation.
3. Intracoronary Anticoagulants
Investigational therapies including local delivery of antithrombotic agents aim to minimize systemic exposure and bleeding risk while targeting thrombus formation directly.
Personalized Risk Stratification and Adjunct Selection
The selection of adjunctive therapies during PCI should be based on a careful balance of thrombotic and bleeding risks.
Risk Stratification Tools
- PRECISE-DAPT: Assesses bleeding risk
- DAPT Score: Determines benefit vs. risk of prolonged dual antiplatelet therapy
- GRACE and TIMI scores: For ischemic risk evaluation in ACS
Tailored Approaches
| Patient Profile | Recommended Adjunct Strategy |
|---|---|
| STEMI with visible thrombus | DAPT + GP IIb/IIIa inhibitors ± thrombus aspiration |
| High bleeding risk | Short-duration DAPT + bivalirudin |
| Prior stroke or elderly | Avoid prasugrel; prefer clopidogrel or ticagrelor |
| PCI without oral P2Y12 loading | Cangrelor bridging + aspirin |
| Saphenous vein graft PCI | Use distal protection device + DAPT |
Clinical Outcomes and Guideline Recommendations
Clinical Trials Supporting Adjunct Use
- PLATO Trial: Demonstrated superior outcomes with ticagrelor over clopidogrel
- ISAR-REACT: Evaluated abciximab in elective PCI
- HORIZONS-AMI: Compared bivalirudin vs. heparin + GP IIb/IIIa inhibitors
- CHAMPION PHOENIX: Supported cangrelor’s efficacy during PCI
Guidelines Summary
- ESC and ACC/AHA endorse DAPT for all PCI patients, with adjuncts individualized by clinical presentation.
- Routine use of GP IIb/IIIa inhibitors is no longer recommended but should be considered for bail-out scenarios.
- Thrombus aspiration is not routine but may be beneficial in selected patients.
Complications and Risk Mitigation
While adjunctive therapies improve thrombotic outcomes, they may elevate the risk of bleeding, especially with potent agents or prolonged use.
Complication Prevention Strategies
- Use bleeding risk calculators pre-PCI
- Choose radial access when feasible
- Monitor activated clotting time (ACT) during PCI
- Opt for short-duration or de-escalated DAPT regimens in high-bleeding-risk patients
The prevention of thrombosis during and after PCI demands a multidimensional approach. The selection and timing of adjunctive pharmacologic agents, combined with mechanical strategies and patient-specific risk assessment, are critical to optimizing outcomes. As PCI techniques evolve, so must our application of evidence-based adjunct therapies to mitigate thrombotic events without compromising safety.