Peptostreptococcus species are anaerobic, gram-positive cocci commonly found as part of the normal flora in the oral cavity, gastrointestinal tract, and female genital tract. Despite their commensal nature, these organisms can become opportunistic pathogens, particularly in the anaerobic environments created by pelvic infections. In pelvic inflammatory disease (PID), Peptostreptococcus spp. play a crucial role in complex polymicrobial infections, often associated with severe inflammatory responses, abscess formation, and long-term reproductive consequences.
Pathogenesis of Anaerobic PID Due to Peptostreptococcus
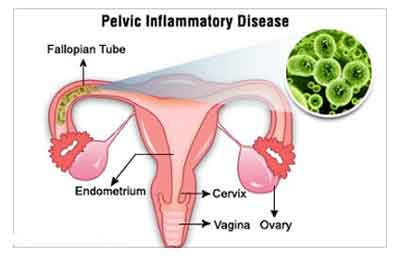
Pelvic inflammatory disease involves infection of the upper female reproductive tract, including the uterus, fallopian tubes, and ovaries. The condition frequently results from the ascending spread of vaginal or cervical microbes into sterile upper genital structures. Peptostreptococcus spp., as anaerobic pathogens, thrive in the hypoxic environments created by necrosis, abscesses, and inflammation. These organisms contribute to tissue destruction and prolonged infection duration.
Risk Factors for Peptostreptococcus PID
Several predisposing factors increase susceptibility to Peptostreptococcus-related pelvic infections:
- Multiple sexual partners and unprotected intercourse
- Intrauterine device (IUD) use
- Prior episodes of PID
- Recent gynecologic procedures (e.g., endometrial biopsy, curettage)
- Postpartum or post-abortion status
- Immunocompromised state (e.g., HIV, diabetes)
Clinical Manifestations of Peptostreptococcus PID
Symptoms are often nonspecific but tend to include both local and systemic signs of infection. Due to the anaerobic nature of Peptostreptococcus, these infections may present more indolently yet progress to severe disease if not promptly treated.
Common Symptoms
- Lower abdominal and pelvic pain
- Abnormal vaginal discharge (often purulent and foul-smelling)
- Dyspareunia (pain during intercourse)
- Irregular menstruation or menorrhagia
- Fever and chills in moderate to severe infections
- Adnexal tenderness and cervical motion tenderness on pelvic examination
Diagnostic Evaluation
Timely and accurate diagnosis is essential to prevent long-term complications such as infertility, ectopic pregnancy, or chronic pelvic pain.
Physical Examination
- Pelvic tenderness, particularly in the adnexal region
- Rebound tenderness in severe cases
- Cervical motion tenderness
Laboratory Investigations
- CBC: Leukocytosis with neutrophilia
- ESR/CRP: Elevated inflammatory markers
- Endocervical and vaginal swabs: Culture for anaerobes including Peptostreptococcus
- Nucleic acid amplification tests (NAATs): Rule out concurrent STIs (e.g., Chlamydia, Gonorrhea)
Imaging Studies
- Transvaginal Ultrasound: Detection of tubo-ovarian abscesses or hydrosalpinx
- Pelvic MRI or CT: For evaluating extensive abscesses, pelvic fluid collections, and inflammatory spread
- Laparoscopy: Definitive diagnosis in unclear or treatment-resistant cases
Microbiology of Peptostreptococcus in PID
Peptostreptococcus spp. often coexist with other anaerobic and facultative organisms, including:
- Bacteroides fragilis
- Prevotella spp.
- Gardnerella vaginalis
- Escherichia coli
- Mycoplasma hominis
- Chlamydia trachomatis and Neisseria gonorrhoeae (co-infective pathogens)
Their role in synergistic infections complicates treatment, often necessitating broad-spectrum therapy until cultures guide specific targeting.
Treatment Protocols for Peptostreptococcus PID
Effective management of PID with anaerobic involvement requires prompt, broad-spectrum antimicrobial therapy, with a focus on anaerobe coverage.
Empiric Antibiotic Regimens
- IV Cefoxitin + Doxycycline
- Clindamycin + Gentamicin
- Ampicillin-Sulbactam + Doxycycline
- Metronidazole (oral or IV) – specifically targets anaerobic flora including Peptostreptococcus
Oral Step-Down Therapy
- Doxycycline + Metronidazole for 14 days following initial IV therapy
Surgical Intervention
Required in cases of:
- Unresponsive tubo-ovarian abscess
- Rupture risk
- Persistent severe infection despite medical management
Procedures may include laparoscopic drainage, salpingo-oophorectomy, or hysterectomy in advanced disease.
Prognosis and Long-Term Outcomes
Timely intervention results in favorable outcomes for most patients. However, delayed diagnosis or inadequate treatment increases the risk of:
- Chronic pelvic pain
- Fallopian tube scarring and infertility
- Increased risk of ectopic pregnancy
- Recurrent PID episodes
Preventive Strategies
To reduce the incidence of Peptostreptococcus-related PID, we must implement the following:
- Routine screening and treatment for STIs in sexually active individuals
- Contraceptive counseling, particularly regarding IUDs and risk mitigation
- Aseptic techniques during gynecologic procedures
- Timely treatment of lower genital tract infections before they ascend
- Partner management and education in sexually transmitted cases
Peptostreptococcus pelvic inflammatory disease represents a complex clinical entity requiring high clinical suspicion, especially in cases unresponsive to typical STI regimens. The anaerobic nature of these infections demands appropriate diagnostic tools and targeted antimicrobial therapy. Awareness, prompt treatment, and preventive strategies are essential to safeguard reproductive health and prevent long-term sequelae.