Peptostreptococcus species are anaerobic, gram-positive cocci that naturally inhabit the female genital tract, gastrointestinal system, and oral cavity. While generally harmless in their native environments, they become significant pathogens when they gain access to normally sterile pelvic tissues. Infections involving Peptostreptococcus spp., particularly pelvic cellulitis, are often polymicrobial and can result in severe complications if left untreated.
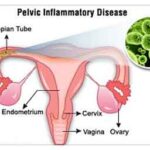
Pelvic cellulitis refers to a diffuse inflammation of the pelvic soft tissue, frequently arising from gynecologic surgeries, childbirth, intrauterine device use, or complications from pelvic inflammatory disease (PID). When Peptostreptococcus is involved, the infection tends to progress under low-oxygen conditions, demanding specific diagnostic and therapeutic approaches.
Etiology and Risk Factors of Peptostreptococcus Pelvic Cellulitis
Anaerobic Pathogenesis
Peptostreptococcus thrives in oxygen-poor environments. When pelvic tissue integrity is compromised—due to trauma, surgery, abscess rupture, or ischemia—anaerobic bacteria colonize the area, triggering an inflammatory cascade and infection spread.
Common Risk Factors
- Postpartum endometritis
- Post-surgical pelvic infections (e.g., hysterectomy, C-section)
- Pelvic inflammatory disease
- Ruptured tubo-ovarian abscess
- Intrauterine device (IUD)-related complications
- Immunosuppression (HIV, corticosteroids, chemotherapy)
- Diabetes mellitus
Clinical Presentation and Symptoms
The presentation of Peptostreptococcus pelvic cellulitis is often subtle initially but can escalate rapidly.
Typical Clinical Features
- Lower abdominal or pelvic pain
- Fever and chills
- Pelvic tenderness and guarding
- Vaginal discharge, often foul-smelling
- Dysuria or urinary frequency
- Leukocytosis and elevated inflammatory markers
- General malaise or sepsis in advanced cases
Diagnostic Evaluation of Anaerobic Pelvic Infections
Physical Examination
Pelvic examination often reveals cervical motion tenderness, adnexal tenderness, or palpable masses. Signs of systemic toxicity, including tachycardia and hypotension, indicate advanced infection.
Laboratory Investigations
- CBC: Elevated white blood cell count.
- C-reactive protein (CRP) and ESR: Markedly raised.
- Blood cultures: May reveal anaerobic bacteremia, though often negative.
- High vaginal and endocervical swabs: Anaerobic cultures necessary to isolate Peptostreptococcus spp.
Imaging Studies
- Ultrasound (Transvaginal/Transabdominal): First-line imaging to detect abscesses or fluid collections.
- CT or MRI Pelvis: Offers superior delineation of soft tissue planes, abscesses, and cellulitis spread.
Management and Treatment Strategy
Empirical and Targeted Antimicrobial Therapy
Prompt initiation of broad-spectrum antimicrobial therapy is essential, covering both anaerobic and aerobic organisms until culture results allow narrowing.
First-Line Antibiotics:
- Clindamycin – Effective against anaerobes, excellent pelvic tissue penetration.
- Metronidazole – Highly active against anaerobic bacteria; often used in combination.
- Beta-lactam/beta-lactamase inhibitors (e.g., ampicillin-sulbactam, piperacillin-tazobactam)
- Cefoxitin or cefotetan – Commonly used in gynecologic infections.
Duration:
- Uncomplicated cellulitis: 10–14 days
- Abscess or surgical site involvement: 2–4 weeks with possible IV-to-oral switch
Surgical Intervention
Surgical management is necessary if abscesses or extensive necrotic tissue are present.
- Drainage of pelvic abscesses (percutaneous or laparoscopic)
- Debridement of necrotic tissue
- Hysterectomy or salpingo-oophorectomy in severe or recurrent infections
Complications of Untreated or Resistant Pelvic Cellulitis
Without prompt and appropriate therapy, Peptostreptococcus pelvic cellulitis can lead to significant morbidity.
Notable Complications
- Tubo-ovarian abscess
- Peritonitis
- Septic pelvic thrombophlebitis
- Infertility due to fallopian tube damage
- Chronic pelvic pain
- Sepsis and multi-organ failure
Preventive Measures in High-Risk Populations
- Antibiotic Prophylaxis during pelvic surgeries
- Proper Aseptic Technique in IUD insertion or gynecologic procedures
- Early Treatment of Vaginal or Cervical Infections
- Glycemic Control in diabetic patients
- Avoidance of Unnecessary Vaginal Instrumentation
Prognosis and Follow-Up
With appropriate antibiotic therapy and, when required, surgical intervention, the prognosis is favorable. Delays in treatment, especially in immunocompromised individuals, increase the risk of adverse outcomes.
Follow-Up Protocols
- Repeat imaging to confirm resolution of abscess or cellulitis
- Monitoring of inflammatory markers
- Gynecologic evaluation to assess anatomical and fertility complications
- Counseling and partner evaluation in sexually transmitted cases
Peptostreptococcus pelvic cellulitis is a serious but manageable condition that necessitates early recognition, anaerobic-targeted antibiotic therapy, and often, surgical drainage or debridement. Effective collaboration between gynecology, infectious diseases, and surgical teams ensures improved patient outcomes, reduces recurrence, and prevents long-term complications.