Peptostreptococcus liver abscess is a clinically important yet frequently under-recognized form of pyogenic hepatic abscess caused by gram-positive anaerobic cocci of the Peptostreptococcus genus. These bacteria are normally part of the commensal flora of mucosal surfaces but can act opportunistically, leading to severe intra-abdominal infections, particularly in the liver, under certain conditions.
Liver abscesses develop when pathogens infiltrate hepatic tissue, leading to necrosis, suppuration, and the formation of purulent cavities. The anaerobic environment of necrotic hepatic tissue provides an ideal niche for Peptostreptococcus spp., especially in polymicrobial infections.

Pathogenesis of Peptostreptococcus-Induced Liver Abscess
Mechanisms of Entry and Infection
The liver may become infected by Peptostreptococcus via:
- Biliary tract infections (e.g., ascending cholangitis)
- Portal vein bacteremia from gastrointestinal sources
- Hematogenous spread through systemic circulation
- Direct extension from adjacent infected structures
- Post-surgical contamination or trauma
Once lodged in the hepatic tissue, Peptostreptococcus incites an inflammatory cascade, resulting in tissue necrosis, pus formation, and encapsulated abscess development.
Epidemiology and Risk Factors
Although aerobic organisms are more commonly implicated in hepatic abscesses, anaerobes, especially Peptostreptococcus, are increasingly recognized due to improved diagnostic techniques. This pathogen is often found in polymicrobial infections, coexisting with Enterobacteriaceae, Bacteroides spp., or Fusobacterium.
Risk factors include:
- Biliary tract disease (e.g., stones, strictures, malignancy)
- Recent gastrointestinal or hepatobiliary surgery
- Immunosuppression (HIV, corticosteroids, chemotherapy)
- Diabetes mellitus
- Intra-abdominal sepsis or appendicitis
- Colorectal cancer or diverticulitis
Clinical Features and Symptoms
Peptostreptococcus liver abscess often presents with non-specific, subacute symptoms, making early diagnosis difficult. The classical triad of fever, right upper quadrant pain, and hepatomegaly is observed in many cases.
Additional signs include:
- Chills and rigors
- Anorexia and weight loss
- Nausea and vomiting
- Jaundice (in biliary involvement)
- Tender hepatomegaly on examination
- Elevated liver enzymes (ALT, AST, ALP) and bilirubin
Symptoms may persist for weeks due to the insidious onset typical of anaerobic infections.
Diagnostic Evaluation
Laboratory Investigations
- Complete Blood Count (CBC): Leukocytosis with neutrophilic predominance
- Liver Function Tests: Elevated transaminases and alkaline phosphatase
- Blood Cultures: May be positive in 20–50% but often negative for anaerobes
- Inflammatory Markers: Elevated ESR and C-reactive protein
Imaging Studies
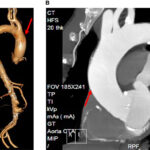
- Ultrasound: First-line imaging; reveals hypoechoic or complex cystic lesions
- Contrast-Enhanced CT Scan: Superior for abscess localization, size, and guiding drainage
- MRI with contrast: Useful in distinguishing abscess from tumors or cysts
Microbiological Analysis
- Needle Aspiration or Drainage Culture: Essential for detecting anaerobes
- Cultures must be processed under strict anaerobic conditions
- Molecular methods like 16S rRNA sequencing enhance detection of Peptostreptococcus spp.
Microbiology and Characteristics of Peptostreptococcus
- Gram-positive anaerobic cocci, non-motile and non-spore forming
- Commonly part of polymicrobial infections
- Major species include Peptostreptococcus anaerobius, P. micros, and Finegoldia magna (formerly P. magnus)
- Identified via anaerobic culture, MALDI-TOF, or PCR-based sequencing
Treatment of Peptostreptococcus Liver Abscess
Effective treatment requires a combination of antibiotic therapy and abscess drainage. Delays in intervention may lead to rupture, sepsis, or multiorgan failure.
Antimicrobial Therapy
Initial empiric therapy must cover anaerobes and common facultative gram-negative rods.
Recommended regimens include:
- Ampicillin-sulbactam IV
- Piperacillin-tazobactam IV
- Metronidazole + 3rd gen cephalosporin (e.g., ceftriaxone)
- Carbapenems for severe or resistant infections
Definitive therapy should be guided by culture sensitivity. Most Peptostreptococcus spp. are sensitive to:
- Penicillin
- Clindamycin
- Metronidazole
- Beta-lactam/beta-lactamase inhibitors
Duration: 4 to 6 weeks, often beginning with intravenous therapy followed by oral antibiotics.
Percutaneous or Surgical Drainage
- Percutaneous needle aspiration: Suitable for small, unilocular abscesses
- Percutaneous catheter drainage: Standard for abscesses >3–5 cm
- Surgical drainage: Reserved for multiloculated or ruptured abscesses, or failed percutaneous approach
Prognosis and Complications
When diagnosed early and managed appropriately, prognosis is favorable, with high recovery rates. However, delayed diagnosis or inadequate drainage can lead to complications:
- Septic shock
- Peritonitis from abscess rupture
- Empyema if spread to pleural cavity
- Chronic liver abscess formation
- Death in untreated or immunocompromised patients
Prevention and Risk Reduction
- Prompt treatment of intra-abdominal infections
- Prophylactic antibiotics in high-risk surgical procedures
- Biliary drainage in obstructive disease
- Careful aseptic technique during liver biopsies or catheterizations
Peptostreptococcus liver abscess, though rare, represents a serious form of anaerobic intra-abdominal infection. Clinicians must maintain high suspicion in at-risk patients presenting with subacute liver-related symptoms. Rapid imaging, anaerobic cultures, and timely combined medical-surgical management significantly reduce morbidity and mortality. Advances in anaerobic diagnostics now allow earlier and more accurate identification of Peptostreptococcus spp., enabling tailored antimicrobial regimens and improved patient outcomes.