Peptostreptococcus, a genus of anaerobic, gram-positive cocci, forms part of the normal flora of the female genital tract. However, under specific pathological conditions, particularly those involving compromised uterine integrity or post-procedural contamination, it emerges as a key pathogen in bacterial endometritis.
Endometritis, the inflammation of the endometrial lining, becomes particularly concerning when Peptostreptococcus is involved due to its synergy with other anaerobes and facultative bacteria, leading to polymicrobial pelvic infections and escalating the risk of chronic pelvic inflammatory disease (PID), infertility, or sepsis
Etiology: How Peptostreptococcus Causes Endometritis
Disruption of Uterine Defense Mechanisms
Peptostreptococcus exploits conditions where the cervix is dilated, uterine flora is disturbed, or post-procedural entry facilitates anaerobic proliferation. This includes:
- Postpartum endometritis
- Post-abortion sepsis
- IUD-related infections
- After gynecologic surgeries (e.g., dilation and curettage)
Synergistic Polymicrobial Growth
Peptostreptococcus often coexists with Bacteroides fragilis, Prevotella, and Gardnerella vaginalis, forming anaerobic biofilms that protect pathogens from antibiotics and immune responses. This polymicrobial synergy results in persistent uterine inflammation, leading to adhesion formation and tubal damage.
Clinical Manifestations of Peptostreptococcus-Induced Endometritis
Symptoms can range from mild to severe depending on the bacterial load, patient’s immune response, and co-infection status:
- Lower abdominal pain and cramping
- Purulent or foul-smelling vaginal discharge
- Fever (≥38°C) and chills
- Uterine tenderness on bimanual examination
- Abnormal uterine bleeding or prolonged lochia
- In severe cases, systemic signs of sepsis
These symptoms may emerge within 48 to 72 hours post-intervention or postpartum, especially if anaerobic pathogens like Peptostreptococcus are involved.
Diagnostic Approach: Identifying Anaerobic Uterine Infections
Laboratory Evaluation
- CBC: Elevated white blood cell count with neutrophilia
- CRP and ESR: Markedly raised in acute inflammation
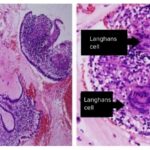
- Endometrial biopsy/culture: Isolation of Peptostreptococcus via anaerobic culture
- Gram stain: Shows gram-positive cocci in chains
Imaging Techniques
1. Transvaginal Ultrasound
- Detects intrauterine collections or retained products of conception (RPOC)
2. MRI or CT Scan
- Used in complicated cases to evaluate the extent of pelvic inflammatory disease or abscess formation
Microbiology and Resistance Patterns
Characteristics of Peptostreptococcus
- Gram-positive anaerobic cocci
- Non-spore forming
- Often found in polymicrobial uterine cultures
- Produces beta-lactamase in some strains
Antimicrobial Resistance Trends
- Resistant to macrolides and tetracyclines
- Variable susceptibility to clindamycin
- High susceptibility to beta-lactam/beta-lactamase inhibitors, metronidazole, and carbapenems
Prompt and appropriate antibiotic selection is critical to avoid treatment failure due to resistant strains.
Treatment Strategies for Peptostreptococcus Endometritis
Empirical Antibiotic Therapy
Initial treatment must target both aerobic and anaerobic flora. Effective regimens include:
- Clindamycin + Gentamicin
- Ampicillin-sulbactam
- Ceftriaxone + Metronidazole
- Piperacillin-tazobactam for broader coverage in severe cases
Duration of treatment ranges from 10 to 14 days, adjusted based on clinical response and culture results.
Surgical Intervention
- Uterine evacuation in cases with retained products
- Drainage of abscesses if pelvic collections are present
- Removal of intrauterine devices when implicated in infection
Complications and Prognostic Concerns
If not managed promptly, Peptostreptococcus-related endometritis may progress to:
- Pelvic abscesses
- Tubo-ovarian abscess formation
- Infertility due to fallopian tube scarring
- Septicemia or septic shock
Early recognition and appropriate therapy result in a favorable prognosis. However, delayed or inadequate treatment may lead to long-term reproductive consequences.
Preventive Strategies and Clinical Recommendations
- Sterile technique during gynecologic procedures
- Prophylactic antibiotics for high-risk intrauterine manipulations
- Prompt removal of retained products of conception
- Regular monitoring in postpartum women and those with IUDs
Peptostreptococcus is a critical pathogen in the pathogenesis of complicated bacterial endometritis, particularly in polymicrobial contexts. Its anaerobic nature and resistance profile necessitate a deliberate, evidence-based approach to diagnosis, antimicrobial therapy, and potential surgical management. Comprehensive care not only resolves infection but also prevents pelvic inflammatory sequelae, ensuring preservation of reproductive health.