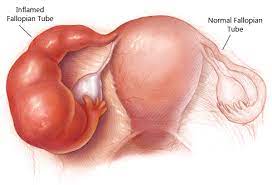
Peptococcus species are anaerobic gram-positive cocci that inhabit various mucosal surfaces, including the gastrointestinal and genitourinary tracts. While typically part of the commensal flora, they may become pathogenic under certain conditions. One such critical condition is the formation of a tubo-ovarian abscess (TOA)—a serious complication often arising from pelvic inflammatory disease (PID).
Tubo-ovarian abscesses are encapsulated infectious masses involving the fallopian tube, ovary, and adjacent pelvic structures. When caused by Peptococcus, the infection typically represents a polymicrobial anaerobic invasion, demanding immediate medical attention.
Etiology: Understanding the Anaerobic Pathogenesis
Polymicrobial Synergy in TOA
The pathogenesis of TOA often involves a combination of aerobic and anaerobic organisms. Peptococcus, particularly in combination with Bacteroides fragilis, Prevotella, or Escherichia coli, plays a significant role in forming resilient and necrotizing infections. Anaerobes such as Peptococcus thrive in ischemic environments, especially post-gynecological procedures, intrauterine device (IUD) usage, or secondary to PID.
Risk Factors
- History of pelvic inflammatory disease
- Multiple sexual partners
- Previous gynecologic surgeries
- Use of intrauterine contraceptive devices
- Immunocompromised status
Clinical Presentation: Symptoms of Peptococcus TOA
Patients with Peptococcus-induced TOA typically present with subacute to acute pelvic symptoms:
- Severe lower abdominal pain
- High-grade fever with chills
- Abnormal vaginal discharge
- Menstrual irregularities
- Dyspareunia (painful intercourse)
- Malaise and anorexia
In cases of abscess rupture, signs of peritonitis and sepsis may develop, necessitating emergency intervention.
Diagnostic Approach: Imaging and Laboratory Investigations
Laboratory Markers
- Complete Blood Count (CBC): Elevated white blood cell count with neutrophilia
- C-Reactive Protein (CRP) and ESR: Indicative of acute inflammation
- Microbial Culture and Gram Stain: Identification of anaerobic cocci (Peptococcus) from aspirated fluid
Imaging Modalities
1. Transvaginal Ultrasound (TVUS)
- First-line diagnostic tool
- Reveals complex adnexal masses with thick walls and internal septations
2. Pelvic MRI or CT Scan
- Confirms extent of abscess
- Assesses for rupture or involvement of adjacent pelvic organs
Management Strategies for Peptococcus-Related TOA
Medical Management
Initial treatment involves broad-spectrum intravenous antibiotics targeting both anaerobic and aerobic organisms.
Recommended Regimens:
- Cefoxitin or Cefotetan + Doxycycline
- Clindamycin + Gentamicin
- Metronidazole for enhanced anaerobic coverage
Treatment duration typically spans 14 to 21 days, with monitoring of clinical response.
Interventional and Surgical Options
In cases where medical therapy fails or the abscess size exceeds 8 cm, further interventions are necessary:
- Image-guided drainage via ultrasound or CT
- Laparoscopic or open surgical drainage
- Salpingo-oophorectomy in refractory or ruptured abscesses
Complications of Untreated or Delayed TOA
Peptococcus-associated TOAs, if not promptly diagnosed and treated, may lead to serious consequences:
- Infertility due to tubal damage
- Chronic pelvic pain
- Peritonitis and intra-abdominal sepsis
- Adhesion formation
- Ectopic pregnancy
Prognosis and Follow-Up
With timely intervention, most patients recover without lasting sequelae. Follow-up includes:
- Reassessment via ultrasound to confirm resolution
- Monitoring for PID recurrence
- Counseling regarding safe sexual practices and contraceptive methods
Prevention Strategies
- Early diagnosis and treatment of pelvic inflammatory disease
- Limiting the use of intrauterine devices in high-risk individuals
- Routine gynecological checkups
- Educating patients on symptoms of pelvic infections
Peptococcus tubo-ovarian abscess represents a complex and potentially life-threatening gynecological infection requiring a multidisciplinary approach. Recognition of early signs, accurate imaging, and prompt initiation of antibiotic therapy are essential to prevent complications such as infertility and sepsis. In the presence of abscess enlargement or failure to respond to conservative therapy, surgical management ensures definitive treatment and reduces the risk of recurrence.