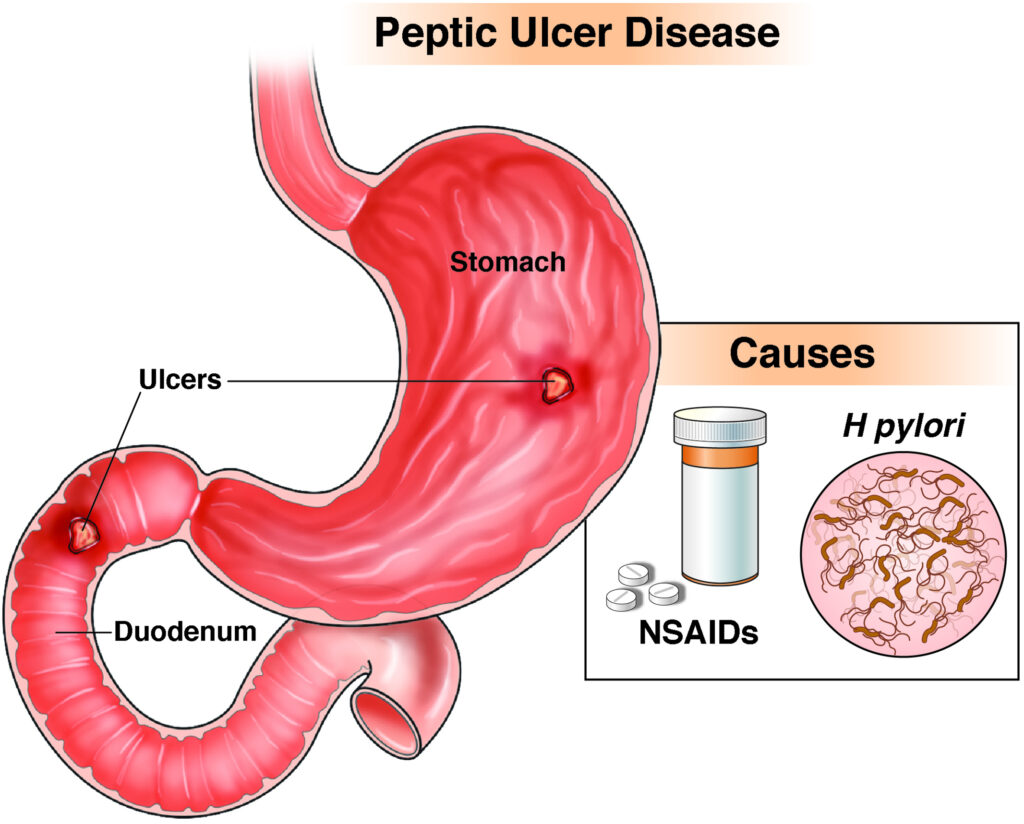
A peptic ulcer refers to an open sore or lesion that develops in the mucosal lining of the stomach or duodenum due to the corrosive action of gastric acid and pepsin. These ulcers can cause significant discomfort and lead to severe complications if not treated promptly.
There are two primary types:
- Gastric Ulcers: Located in the stomach lining
- Duodenal Ulcers: Occur in the upper portion of the small intestine (duodenum)
Etiology: Common Causes of Peptic Ulcer Disease
The delicate balance between aggressive factors (like acid, pepsin) and protective mechanisms (mucus, bicarbonate, prostaglandins) in the gastrointestinal tract determines mucosal integrity. Disruption of this balance leads to ulcer formation.
Major Contributing Factors:
- Helicobacter pylori Infection
This gram-negative bacterium colonizes the gastric mucosa, inducing chronic inflammation and mucosal damage. H. pylori is detected in up to 90% of duodenal and 70% of gastric ulcer cases. - Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Chronic NSAID usage impairs prostaglandin synthesis, weakening mucosal defenses and predisposing to ulceration. - Stress and Critical Illness (Stress Ulcers)
Severe physiological stress from trauma, burns, or sepsis can precipitate ulcer formation in critically ill patients. - Lifestyle Factors
Smoking, excessive alcohol consumption, and high caffeine intake exacerbate mucosal injury and delay healing. - Zollinger-Ellison Syndrome
A rare condition where gastrin-secreting tumors cause hypersecretion of gastric acid.
Pathophysiology of Peptic Ulcers
The progression of a peptic ulcer involves an interplay of host immune response, bacterial virulence factors (e.g., CagA, VacA proteins in H. pylori), and environmental triggers.
Over time, the ulcer can penetrate deeper layers, potentially causing hemorrhage, perforation, or gastric outlet obstruction.
Clinical Presentation: Signs and Symptoms of Peptic Ulcers
Ulcers may present with a variety of gastrointestinal complaints, or remain asymptomatic in early stages.
Typical Symptoms:
- Epigastric pain: Burning, gnawing sensation, often relieved or worsened by meals
- Bloating and fullness
- Nausea and occasional vomiting
- Belching and indigestion
- Weight loss in severe cases
- Dark, tarry stools (melena) indicating gastrointestinal bleeding
Complications of Untreated Peptic Ulcers
Failure to diagnose and treat ulcers can lead to life-threatening complications:
- Bleeding: The most common complication, leading to anemia or hemorrhagic shock
- Perforation: Sudden onset of severe abdominal pain, indicating perforation into the peritoneal cavity
- Penetration: Ulcer invades adjacent organs like the pancreas or liver
- Gastric Outlet Obstruction: Chronic inflammation and scarring cause narrowing of the pyloric canal, leading to vomiting and weight loss
Diagnostic Approach for Peptic Ulcer Disease
An accurate diagnosis is essential to differentiate peptic ulcers from other gastrointestinal disorders and to identify underlying causes.
Primary Diagnostic Tools:
- Upper Gastrointestinal Endoscopy (EGD)
Gold standard for direct visualization, biopsy, and ruling out malignancy - H. pylori Testing
- Urea breath test
- Stool antigen test
- Rapid urease test (CLO test)
- Histological examination of biopsy
- Barium Swallow X-ray: Less commonly used; highlights crater-like defects
- Laboratory Tests:
- Hemoglobin (to detect anemia)
- Occult blood test in stool
- Serum gastrin levels in suspected Zollinger-Ellison syndrome
Evidence-Based Treatment Options
The goal of treatment is to eradicate H. pylori, neutralize gastric acid, and protect the mucosa to allow healing.
1. Eradication of H. pylori Infection
Triple Therapy (14 days):
- Proton Pump Inhibitor (PPI)
- Clarithromycin
- Amoxicillin or Metronidazole
Quadruple Therapy:
- PPI
- Bismuth subsalicylate
- Metronidazole
- Tetracycline
2. Acid Suppression Therapy
- Proton Pump Inhibitors (PPIs): Omeprazole, Pantoprazole – inhibit acid secretion
- H2-Receptor Antagonists: Ranitidine, Famotidine – less potent than PPIs
- Antacids: Provide symptomatic relief by neutralizing gastric acid
- Sucralfate and Misoprostol: Enhance mucosal defense and aid in healing
3. Management of NSAID-Induced Ulcers
- Discontinue or reduce NSAID usage
- Initiate PPI therapy
- Consider switching to selective COX-2 inhibitors if NSAIDs are necessary
Surgical Intervention
Surgery is reserved for patients with:
- Non-healing ulcers
- Complications like perforation, bleeding, or obstruction
- Suspicion of malignancy in gastric ulcers
Surgical options include vagotomy, antrectomy, or partial gastrectomy depending on the ulcer location and severity.
Prognosis and Healing Rates
With appropriate treatment:
- H. pylori eradication results in >90% ulcer healing rate
- NSAID-induced ulcers heal within 6–8 weeks with PPI therapy
- Recurrence is significantly reduced after complete eradication of H. pylori
Prevention and Long-term Management
Key Preventive Strategies:
- Avoid prolonged NSAID use unless medically necessary
- Test and treat H. pylori in high-risk individuals
- Smoking cessation and alcohol moderation
- Stress management and dietary modification
- Long-term acid suppression in high-risk or recurrent cases
Peptic ulcer disease remains a common and manageable condition with the potential for serious complications if neglected. A comprehensive diagnostic and therapeutic approach—centered around H. pylori eradication, acid suppression, and lifestyle modification—ensures high rates of healing and minimizes recurrence. Vigilance in diagnosis and adherence to treatment protocols are vital to gastrointestinal health and patient outcomes.