Unilateral amblyopia, commonly referred to as “lazy eye,” is a neurodevelopmental visual disorder characterized by reduced best-corrected visual acuity in one eye, not attributable to any structural abnormality. It typically arises due to strabismus, anisometropia, or visual deprivation during the critical period of visual development.
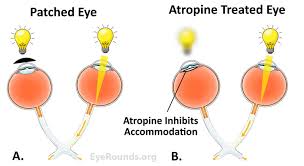
While occlusion therapy (patching) remains the most widely recognized treatment, penalization therapy has emerged as an effective and often better-tolerated alternative for many patients, especially children.
What Is Penalization Therapy?
Penalization therapy involves functionally impairing the better-seeing eye to stimulate visual development in the amblyopic eye. Unlike patching, penalization does not require physical occlusion but instead uses optical or pharmacologic interventions to blur vision in the dominant eye.
Types of Penalization Therapy for Amblyopia
Penalization can be categorized based on the method and frequency of application. Each modality has specific indications depending on age, severity, and etiology of amblyopia.
1. Pharmacologic Penalization (Atropine)
- Mechanism: Atropine sulfate (1%) induces cycloplegia and mydriasis, blurring near vision in the sound eye.
- Application: Typically instilled once daily or on alternate days.
- Effectiveness: Best suited for moderate amblyopia (20/40 to 20/100) in children aged 3–7 years.
2. Optical Penalization
- Mechanism: Use of plus lenses, diffusing filters, or frosted spectacles to degrade the image quality in the sound eye.
- Advantages: Non-invasive and better tolerated than patching.
- Limitations: Requires precise refractive correction and compliance with lens wear.
3. Total vs. Partial Penalization
| Type | Description |
|---|---|
| Total | Blurring both distance and near vision in the sound eye |
| Partial | Selectively blurring near or distance only |
| Alternating | Switching penalization between eyes to prevent reverse amblyopia |
Mechanism of Action of Penalization Therapy
Penalization promotes use-dependent plasticity in the amblyopic eye. By reducing the visual input of the dominant eye, the brain is compelled to process input from the weaker eye, thus enhancing visual acuity and cortical responsiveness.
Clinical Evidence Supporting Penalization Therapy
Amblyopia Treatment Studies (ATS)
The Pediatric Eye Disease Investigator Group (PEDIG) conducted several randomized controlled trials:
- ATS-1: Found daily atropine penalization to be as effective as patching for moderate amblyopia in children aged 3 to 7.
- ATS-2B: Demonstrated weekend atropine was nearly as effective as daily atropine, improving compliance and reducing side effects.
- ATS-3: Evaluated atropine in older children (7–12 years), showing limited but positive visual gains.
Real-World Application
- Atropine therapy has shown high compliance, particularly in children resistant to patching.
- Optical penalization, such as over-plus lenses, remains widely used in patients intolerant to pharmacologic drops.
Comparison Between Patching and Penalization
| Feature | Patching | Penalization |
|---|---|---|
| Compliance | Lower, due to cosmetic/social issues | Higher, especially with drops |
| Visual Improvement | Slightly faster in severe cases | Comparable in moderate cases |
| Side Effects | Skin irritation, social stigma | Photophobia, reduced near vision |
| Preferred Age Group | Infants and young children | 3–8 years, or non-compliant with patching |
Patient Selection for Penalization Therapy
Ideal Candidates:
- Children aged 3–7 years
- Moderate amblyopia (20/40–20/100)
- Poor compliance with patching
- No contraindications to atropine (e.g., cardiac or neurological disorders)
Contraindications:
- Allergy to atropine
- Narrow-angle glaucoma
- Severe amblyopia (may require initial patching)
Administration Guidelines
Pharmacologic Atropine Use:
- Dose: 1% atropine sulfate, once daily in the sound eye
- Duration: Continued until plateau in visual improvement, usually over 4–6 months
- Monitoring: Regular vision checks every 4–6 weeks
Optical Penalization Techniques:
- Over-plus lenses: +3.00 D to +6.00 D in the sound eye
- Bangerter filters: Graded diffusing filters on spectacle lenses
- Frosted lenses: Completely obscure central vision in the sound eye
Potential Complications and Side Effects
Pharmacologic:
- Photophobia
- Light sensitivity
- Blurred near vision
- Rare systemic effects: dry mouth, fever, tachycardia
Optical:
- Decreased binocular function
- Risk of inducing reverse amblyopia if improperly monitored
Importance of Follow-Up and Monitoring
Frequent follow-up visits are essential to:
- Monitor visual acuity improvement
- Detect reverse amblyopia or side effects
- Adjust therapy as needed, including alternating penalization
- Transition to maintenance therapy or binocular vision training
Emerging Trends in Penalization Therapy
- Binocular therapy integration: Combining penalization with interactive binocular games or virtual reality
- Digital monitoring: Use of mobile apps to track compliance and visual outcomes
- Personalized dosing: Adjusting penalization based on refractive error and visual response
Penalization therapy offers a scientifically supported, non-invasive, and often better-tolerated alternative to patching in the treatment of unilateral amblyopia. Whether through pharmacologic atropine instillation or optical lens manipulation, penalization serves as a powerful tool in the amblyopia management arsenal, especially for children with moderate visual deficits. Optimal outcomes depend on individualized treatment selection, strict follow-up, and consistent compliance, reinforcing the need for a collaborative approach between clinicians, patients, and caregivers.