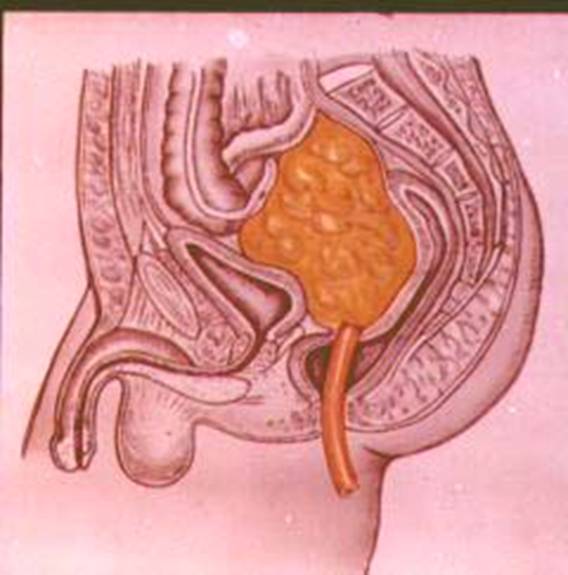
A pelvic abscess is a localized collection of pus within the pelvic cavity, often resulting from a bacterial infection that has spread or remained untreated. This condition can lead to life-threatening complications if not promptly diagnosed and treated. It typically occurs as a sequel to pelvic inflammatory disease (PID), gastrointestinal perforation, or post-surgical infections.
Pathophysiology and Etiology of Pelvic Abscess
Pelvic abscesses form when the immune system walls off infectious material in the pelvis, leading to a pus-filled cavity. Inflammation, necrosis, and tissue destruction follow, which may threaten nearby organs such as the uterus, fallopian tubes, bladder, or intestines.
Common Causes
- Pelvic Inflammatory Disease (PID)
- Tubo-Ovarian Abscess (TOA)
- Postoperative Infections (e.g., after hysterectomy or bowel surgery)
- Perforated Appendicitis
- Diverticulitis
- Crohn’s Disease
- Postpartum infections
Risk Factors
- Multiple sexual partners
- Use of intrauterine devices (IUDs)
- Recent pelvic or abdominal surgery
- History of PID or sexually transmitted infections (STIs)
- Immunocompromised status
- Inflammatory bowel disease
Clinical Presentation: Recognizing Pelvic Abscess Symptoms
Common Symptoms
- Pelvic pain (often severe and unilateral)
- Fever and chills
- Lower abdominal tenderness
- Vaginal discharge
- Dyspareunia (painful intercourse)
- Abnormal uterine bleeding
- Painful urination or defecation
Severe or ruptured abscesses may lead to sepsis, presenting with hypotension, tachycardia, and mental status changes.
Diagnostic Methods for Pelvic Abscess
Prompt diagnosis is crucial to avoid progression to severe systemic infection. A combination of clinical evaluation and imaging studies ensures accuracy.
Clinical Evaluation
- Pelvic examination revealing adnexal tenderness or mass
- Elevated white blood cell count (WBC)
- Increased C-reactive protein (CRP) and ESR
Imaging Techniques
- Transvaginal Ultrasound: First-line tool for visualizing fluid-filled masses
- CT Scan of Abdomen and Pelvis: Superior for detecting size, location, and extension
- MRI: Used in complex cases or during pregnancy
Microbiological Testing
- Endocervical swabs: To identify causative organisms (e.g., Chlamydia trachomatis, Neisseria gonorrhoeae)
- Blood cultures: If systemic infection is suspected
Treatment Modalities for Pelvic Abscess
Treatment depends on the size, cause, and clinical status of the patient.
Medical Management
- Empiric broad-spectrum intravenous antibiotics are initiated:
- Cefoxitin + Doxycycline + Metronidazole
- Alternatives: Clindamycin + Gentamicin
Medical management is suitable for abscesses smaller than 8 cm and in hemodynamically stable patients.
Interventional Drainage
If medical therapy fails or the abscess is large:
- Percutaneous drainage (guided by CT or ultrasound)
- Transvaginal drainage for tubo-ovarian abscesses
Surgical Intervention
Surgical procedures are indicated in the following scenarios:
- Ruptured abscess with generalized peritonitis
- Failure of antibiotic and drainage therapy
- Suspected malignancy
Surgical options include:
- Laparoscopic drainage
- Laparotomy in emergencies
- Hysterectomy or salpingo-oophorectomy if reproductive organs are severely affected
Complications of Untreated Pelvic Abscess
- Sepsis and septic shock
- Chronic pelvic pain
- Infertility
- Ectopic pregnancy
- Peritonitis
- Intestinal obstruction
Early detection and intervention are key to preventing these severe outcomes.
Prognosis and Long-Term Outlook
With prompt diagnosis and adequate therapy, the prognosis is generally favorable. However, delays in treatment can lead to irreversible damage to reproductive organs and increased mortality.
Regular follow-up is essential, especially in patients treated non-surgically, to ensure resolution of the abscess and prevent recurrence.
Preventive Measures
Sexual Health and Hygiene
- Regular STI screening
- Condom use to reduce PID risk
- Avoidance of high-risk sexual behaviors
Postoperative Care
- Adherence to aseptic techniques during pelvic surgeries
- Prophylactic antibiotics when appropriate
Chronic Disease Management
- Timely management of diverticulitis, Crohn’s disease, and appendicitis to avoid pelvic spread
Special Considerations in Pregnancy and Pediatrics
During Pregnancy
Pelvic abscesses pose significant risks during pregnancy, including preterm labor, miscarriage, and fetal infection. MRI is the preferred imaging modality due to radiation concerns.
Pediatric Cases
Rare but possible in adolescent girls, often due to congenital anomalies or complicated appendicitis. Treatment mirrors adult protocols but requires pediatric surgical expertise.
A pelvic abscess is a serious and potentially life-threatening condition demanding immediate medical attention. Understanding its causes, identifying its symptoms early, and employing a multidisciplinary approach to treatment can significantly improve outcomes. Preventive strategies remain vital in reducing incidence, particularly in high-risk groups.