Understanding Benign Prostatic Hyperplasia (BPH)
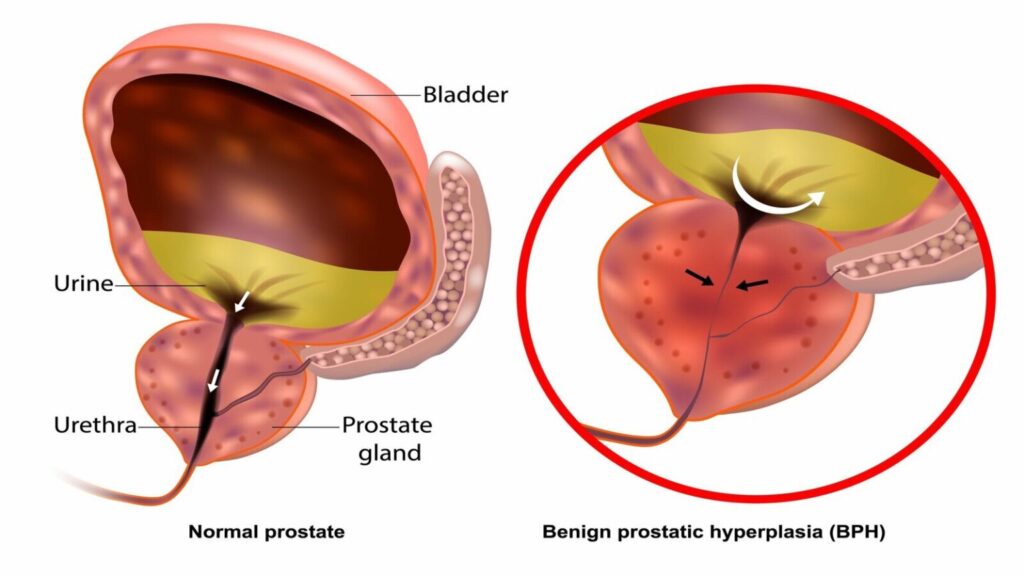
Benign Prostatic Hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland commonly affecting aging men. The condition leads to the compression of the urethra, resulting in lower urinary tract symptoms (LUTS). BPH is one of the most prevalent urological disorders, with its incidence rising significantly after the age of 50.
The Link Between BPH and Lower Urinary Tract Symptoms (LUTS)
Lower urinary tract symptoms (LUTS) refer to a range of urinary issues that can significantly impact quality of life. These symptoms are categorized into two groups:
- Storage Symptoms: Increased frequency, urgency, nocturia (waking at night to urinate).
- Voiding Symptoms: Hesitancy, weak stream, straining, and incomplete bladder emptying.
BPH-induced LUTS occur primarily due to obstruction of urine flow caused by the enlarged prostate and secondary bladder dysfunction.
Causes and Risk Factors
The exact cause of BPH remains unclear, but several factors contribute to its development:
- Age: The likelihood of BPH increases with age.
- Hormonal Changes: An imbalance in testosterone and dihydrotestosterone (DHT) contributes to prostate growth.
- Genetics: A family history of BPH raises the risk.
- Lifestyle Factors: Sedentary lifestyle and obesity may exacerbate the condition.
Symptoms of BPH with LUTS
- Frequent urination, particularly at night (nocturia)
- Difficulty starting urination
- Weak urinary stream
- Sensation of incomplete bladder emptying
- Dribbling at the end of urination
- Incontinence in severe cases
Diagnosis of BPH with LUTS
A thorough evaluation is critical to differentiate BPH from other urological conditions. Common diagnostic procedures include:
- Medical History and Symptom Assessment: Questionnaires like the International Prostate Symptom Score (IPSS).
- Physical Examination: Digital rectal examination (DRE) to assess prostate size and shape.
- Urinalysis: Rule out infections or blood in the urine.
- Prostate-Specific Antigen (PSA): Screening for prostate cancer.
- Imaging: Ultrasound or MRI to evaluate the prostate and bladder.
- Urodynamic Testing: Assess bladder function and urine flow.
Treatment Options for BPH with LUTS
1. Lifestyle Modifications
- Limiting fluid intake before bedtime
- Reducing caffeine and alcohol consumption
- Regular physical activity
2. Medications
- Alpha-Blockers: Relax prostate and bladder neck muscles (e.g., tamsulosin, alfuzosin).
- 5-Alpha Reductase Inhibitors: Reduce prostate size by inhibiting hormonal changes (e.g., finasteride, dutasteride).
- Combination Therapy: Alpha-blockers combined with 5-alpha reductase inhibitors for enhanced effectiveness.
- Anticholinergics: Address overactive bladder symptoms.
3. Minimally Invasive Procedures
- Transurethral Microwave Therapy (TUMT): Heat application to reduce prostate tissue.
- Prostatic Urethral Lift (PUL): Implant placement to hold prostate lobes apart.
- Rezum Water Vapor Therapy: Steam application to destroy prostate cells.
4. Surgical Interventions
- Transurethral Resection of the Prostate (TURP): The gold-standard surgical option for severe cases.
- Laser Therapy: Photoselective vaporization of the prostate (PVP) or Holmium Laser Enucleation of the Prostate (HoLEP).
- Open Prostatectomy: Recommended for very large prostates.
Managing Complications
Untreated Benign prostatic hyperplasia with lower urinary tract may lead to:
- Urinary retention
- Recurrent urinary tract infections (UTIs)
- Bladder stones
- Kidney damage
Timely intervention and regular follow-ups with a urologist are crucial to prevent complications.
Prognosis and Quality of Life
While BPH is not life-threatening, its symptoms can significantly affect quality of life. Most patients experience symptom improvement with appropriate management. Early diagnosis and adherence to treatment plans are key to minimizing long-term impacts.