Hypoglycemia remains one of the most serious acute complications in individuals with diabetes mellitus. It not only impairs immediate physiological function but also contributes significantly to long-term morbidity and treatment non-adherence. Identifying patients at risk of hypoglycemia, understanding its mechanisms, and instituting robust prevention and management strategies are essential to safe and effective diabetes care.
Understanding Hypoglycemia in Diabetes Mellitus
Definition and Clinical Thresholds
Hypoglycemia is defined as a blood glucose concentration below 70 mg/dL (3.9 mmol/L). Clinically significant hypoglycemia often refers to levels under 54 mg/dL (3.0 mmol/L). Severe hypoglycemia is characterized by cognitive impairment requiring external assistance for recovery.
High-Risk Profiles: Patients Susceptible to Hypoglycemia
Identifying Vulnerable Subgroups
Certain individuals with diabetes mellitus exhibit increased susceptibility to hypoglycemic episodes due to physiological, pharmacological, or lifestyle factors:
- Type 1 diabetes mellitus patients using intensive insulin regimens
- Elderly individuals, especially with polypharmacy or cognitive decline
- Chronic kidney disease (CKD) patients with impaired insulin clearance
- Individuals with hypoglycemia unawareness or autonomic neuropathy
- Patients on sulfonylureas or meglitinides
- Recent hospital discharge or recent changes in treatment regimen
Pathophysiological Basis of Hypoglycemia in Diabetic Patients
Hypoglycemia occurs when there is an imbalance between glucose availability and glucose utilization. This imbalance is often the result of excess insulin action or impaired counter-regulatory responses, particularly in insulin-treated diabetes.
Key mechanisms include:
- Iatrogenic insulin excess
- Inadequate caloric intake or delayed meals
- Increased physical activity without adjustment in insulin or food intake
- Alcohol-induced gluconeogenesis suppression
- Reduced renal or hepatic clearance of insulin or oral hypoglycemics
Recognizing Clinical Manifestations of Hypoglycemia
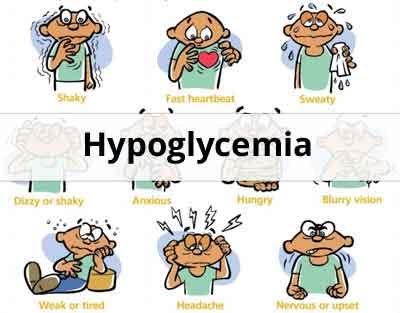
Symptoms and Signs
Symptoms may be autonomic (adrenergic) or neuroglycopenic, often progressing rapidly if unaddressed:
Autonomic Symptoms:
- Sweating
- Palpitations
- Tremors
- Hunger
- Anxiety
Neuroglycopenic Symptoms:
- Confusion
- Difficulty concentrating
- Slurred speech
- Seizures
- Loss of consciousness
In patients with hypoglycemia unawareness, neuroglycopenic symptoms may manifest without preceding adrenergic warnings, increasing the risk of severe episodes.
Diagnostic Evaluation and Monitoring Strategies
Tools and Techniques for Detection
- Self-monitoring of blood glucose (SMBG): Frequent checks to identify trends
- Continuous glucose monitoring (CGM): Offers real-time glucose trends and alarms
- Glycemic logs and symptom diaries: Aid in identifying patterns
- Laboratory evaluation: In recurrent unexplained cases, assessment of insulin, C-peptide, and sulfonylurea levels may be warranted
Immediate Management of Hypoglycemia
Step-by-Step Treatment Protocol
Mild to Moderate Hypoglycemia (Conscious Patient):
- Administer 15-20 grams of fast-acting carbohydrates (e.g., glucose tablets, juice)
- Recheck blood glucose after 15 minutes
- Repeat if levels remain <70 mg/dL
- Follow with long-acting carbohydrate once stabilized
Severe Hypoglycemia (Altered Consciousness):
- Administer glucagon injection (IM/SubQ)
- Alternatively, IV dextrose (D50%) in healthcare settings
- Ensure airway safety and monitor vitals
- Identify and address the precipitating cause post-recovery
Long-Term Prevention Strategies in Diabetes Management
Individualized Care Approaches
- Adjust insulin regimens: Consider long-acting basal analogs with lower hypoglycemia risk
- Review and modify oral medications: Especially sulfonylureas
- Implement CGM devices: Especially in those with frequent episodes
- Dietary planning: Emphasize consistent carbohydrate intake
- Physical activity guidance: Tailor insulin/carbohydrate balance around exercise
- Patient and caregiver education: Recognize early symptoms, emergency response
Behavioral and Psychosocial Considerations
Addressing Hypoglycemia-Related Fear
Recurrent hypoglycemia can lead to fear of insulin, treatment non-compliance, and intentional underdosing. Regular counseling, reassurance, and collaborative care are essential to restore confidence in diabetes management.
Special Considerations for Specific Populations
Pediatric Patients
Children with type 1 diabetes may have erratic eating patterns and activity levels. Parental training and CGM use are critical in early detection and prevention.
Older Adults
Increased risk due to cognitive decline, renal impairment, and delayed symptom recognition. Simplified regimens and less stringent glycemic targets may be warranted.
Pregnant Women
Tighter glucose targets during pregnancy increase hypoglycemia risk. Frequent monitoring and close supervision are necessary to safeguard maternal and fetal outcomes.
Post-Episode Assessment and Follow-Up
Following any hypoglycemic event:
- Document the episode in the medical record
- Evaluate contributing factors
- Revise treatment regimens as needed
- Educate the patient on recurrence prevention strategies
- Schedule follow-up to ensure long-term glycemic safety
Effective management of patients with diabetes mellitus at risk of hypoglycemia demands precision, vigilance, and personalization. By integrating risk stratification, continuous monitoring, prompt intervention, and structured education, we can significantly reduce the frequency and impact of hypoglycemic events, thereby enhancing safety and quality of life in diabetic care.