Pathologic myopia, also known as degenerative or malignant myopia, is a severe form of high myopia characterized by progressive and structural changes to the posterior segment of the eye. These changes include excessive axial elongation, thinning of the retina and choroid, posterior staphyloma, and macular atrophy, all of which contribute to irreversible visual impairment.
Defined by an axial length exceeding 26.5 mm or a refractive error greater than -6.00 diopters, pathologic myopia goes beyond simple refractive error to represent a degenerative ocular condition with significant public health implications.
Etiology and Risk Factors
While the precise cause of pathologic myopia remains multifactorial, a combination of genetic, environmental, and biomechanical factors contribute to its development:
- Genetic predisposition (e.g., mutations in PAX6, SCO2)
- Early-onset myopia with rapid axial elongation
- Intensive near-work activities, especially in childhood
- Urban living environments with reduced outdoor time
- Ethnic predilection, notably in East Asian populations
Children who develop myopia early and progress rapidly are at a heightened risk for transitioning into pathologic myopia during adolescence or adulthood.
Pathophysiology and Structural Changes
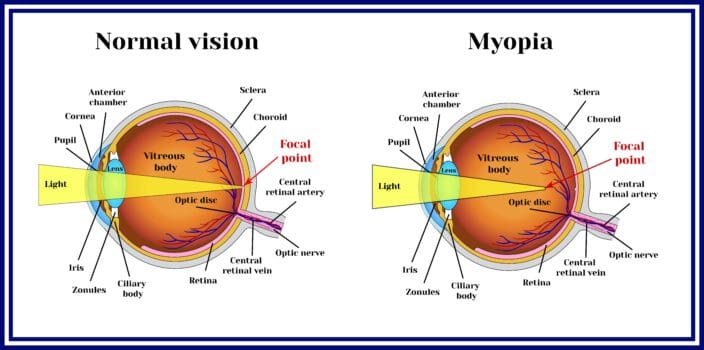
The hallmark of pathologic myopia lies in excessive elongation of the eye’s axial length, leading to mechanical stretching of ocular tissues. This stretching induces degenerative alterations across multiple layers of the posterior segment:
- Sclera: Progressive thinning, particularly at the posterior pole
- Choroid: Marked thinning and atrophy, compromising blood supply
- Retina: Development of lacquer cracks, macular atrophy, and foveoschisis
- Optic disc: Peripapillary atrophy and tilted disc appearance
These structural changes can lead to significant and often irreversible vision loss.
Clinical Features and Symptoms
Pathologic myopia may remain asymptomatic during early stages but often progresses to exhibit the following symptoms:
- Blurred central vision
- Metamorphopsia (distorted vision)
- Scotomas (blind spots)
- Reduced contrast sensitivity
- Progressive decrease in visual acuity
In severe cases, patients may experience legal blindness, particularly when complications such as choroidal neovascularization or retinal detachment occur.
Classification of Myopic Maculopathy
Myopic maculopathy, a key feature of pathologic myopia, is classified according to the META-PM (Myopic Maculopathy Classification):
| Grade | Description |
|---|---|
| 0 | No macular lesions |
| 1 | Tessellated fundus |
| 2 | Diffuse chorioretinal atrophy |
| 3 | Patchy chorioretinal atrophy |
| 4 | Macular atrophy |
| Plus Lesions | Lacquer cracks, CNV, Fuchs spots |
Diagnostic Evaluation of Pathologic Myopia
Imaging and Measurement Techniques
| Diagnostic Tool | Purpose |
|---|---|
| Optical Coherence Tomography (OCT) | Detects macular traction, choroidal thinning, foveoschisis |
| Fundus Photography | Documents macular atrophy, lacquer cracks, staphyloma |
| Axial Length Measurement | Confirms elongation >26.5 mm |
| Fluorescein Angiography (FA) | Identifies choroidal neovascularization |
| Ultra-widefield Imaging | Visualizes peripheral degenerations |
Accurate diagnosis relies on a multimodal imaging approach to assess structural and vascular alterations.
Common Complications of Pathologic Myopia
1. Choroidal Neovascularization (CNV)
Abnormal blood vessels from the choroid invade the retina, causing hemorrhage, scarring, and vision loss. It is one of the leading causes of severe visual decline in pathologic myopia.
2. Retinal Detachment
Due to vitreoretinal traction and posterior staphyloma, individuals are at increased risk for rhegmatogenous retinal detachment, particularly in younger patients.
3. Myopic Foveoschisis
Retinal splitting or schisis due to tractional forces; may lead to foveal detachment if untreated.
4. Macular Atrophy
Chorioretinal degeneration at the central macula causes irreversible loss of fine vision.
5. Posterior Staphyloma
Outward bulging of the posterior sclera distorts normal ocular anatomy and contributes to many of the complications above.
Treatment and Management Strategies
Pharmacological Interventions
- Anti-VEGF Therapy (e.g., Ranibizumab, Aflibercept): First-line treatment for myopic CNV; inhibits abnormal blood vessel growth and stabilizes vision.
- Atropine Eye Drops (low-dose 0.01%): Investigated for slowing myopia progression in children; limited utility in pathologic stages.
Surgical Interventions
- Vitrectomy: Indicated in cases of myopic foveoschisis, macular hole retinal detachment.
- Scleral Reinforcement Surgery: Experimental procedure aimed at strengthening the posterior sclera and halting axial elongation.
Refractive Corrections
- High-index spectacle lenses or specialized contact lenses for optical correction
- Implantable Collamer Lenses (ICL) in non-degenerative high myopia
- Refractive surgery (e.g., LASIK) is contraindicated in pathologic cases due to structural fragility.
Preventive and Lifestyle Measures
Although no definitive cure exists, preventive strategies focus on early intervention and risk mitigation:
- Outdoor activity during childhood: Reduces onset and progression of myopia
- Controlled screen time and near work
- Regular eye examinations in children with myopic parents
- Genetic counseling in families with a history of pathologic myopia
Long-Term Monitoring and Prognosis
Management of pathologic myopia is lifelong and requires routine follow-up with imaging to monitor progression and detect complications early. Prognosis is highly variable:
- Stable vision is possible with early detection and treatment of CNV
- Progressive vision loss may occur despite interventions, especially in cases with macular atrophy or advanced staphyloma
Vision rehabilitation services, including low vision aids and adaptive devices, are essential for patients with significant visual impairment.
Pathologic myopia is a progressive, vision-threatening condition demanding comprehensive clinical attention. Through early diagnosis, multimodal imaging, and timely management of complications such as choroidal neovascularization or retinal detachment, we can significantly mitigate vision loss. With the global prevalence of myopia rising sharply, pathologic myopia is poised to become a leading cause of visual disability. Preventive strategies, coupled with emerging therapeutic innovations, offer hope for improved quality of life for affected individuals.