Patent ductus arteriosus (PDA) is a congenital cardiac anomaly in which the ductus arteriosus—a fetal blood vessel connecting the pulmonary artery to the aorta—fails to close after birth. This persistent opening leads to abnormal circulation between the systemic and pulmonary arteries, resulting in increased workload on the heart and lungs.
During fetal development, the ductus arteriosus diverts blood away from the non-functioning fetal lungs. After birth, this vessel typically closes within the first few hours to days. Failure to do so results in PDA, which can vary in severity depending on the size of the ductus and the infant’s gestational age.
Embryology and Pathophysiology of PDA
The ductus arteriosus is derived from the sixth aortic arch and functions as a vital conduit during intrauterine life. Closure occurs in two phases:
- Functional closure: Within 10–15 hours post-birth due to increased oxygen levels and reduced prostaglandin E2.
- Anatomical closure: Over the next few days, involving fibrous tissue proliferation and permanent sealing.
When this fails, oxygenated blood from the aorta flows back into the pulmonary artery, leading to pulmonary overcirculation and left heart volume overload.
Epidemiology and Risk Factors
PDA accounts for approximately 5–10% of all congenital heart defects, with higher prevalence in:
- Premature infants, especially those <28 weeks gestation
- Females, with a 2:1 female-to-male ratio
- Infants with neonatal respiratory distress syndrome
- High-altitude births, where lower oxygen tension delays closure
- Genetic syndromes such as congenital rubella and trisomy 21
Clinical Presentation and Symptoms
In Neonates and Infants:
- Tachypnea
- Poor feeding
- Failure to thrive
- Continuous “machinery” murmur, best heard at the left upper sternal border
- Bounding pulses and widened pulse pressure
In Older Children and Adults:
- May remain asymptomatic with small PDA
- Large PDA may cause:
- Exercise intolerance
- Fatigue
- Shortness of breath
- Signs of congestive heart failure
- Risk of infective endarteritis
Diagnostic Evaluation of PDA
Physical Examination:
- Characteristic continuous murmur
- Signs of volume overload
Imaging and Tests:
| Diagnostic Tool | Findings |
|---|---|
| Echocardiography | Direct visualization of ductal shunt, chamber enlargement |
| Doppler Ultrasound | Left-to-right shunting |
| Chest X-ray | Cardiomegaly, increased pulmonary vascular markings |
| Electrocardiogram | Left atrial and ventricular enlargement |
| Cardiac MRI/CT | Detailed ductal anatomy in complex cases |
| Cardiac catheterization | Measurement of shunt fraction (Qp/Qs) |
Classification of Patent Ductus Arteriosus
| Type of PDA | Description |
|---|---|
| Silent PDA | No audible murmur; discovered incidentally on imaging |
| Small PDA | Minimal symptoms, audible murmur |
| Moderate PDA | Murmur, mild symptoms like fatigue |
| Large PDA | CHF, respiratory distress, failure to thrive |
Complications of Untreated PDA
- Pulmonary hypertension
- Eisenmenger syndrome (irreversible pulmonary vascular disease)
- Heart failure
- Endocarditis or endarteritis
- Arrhythmias
Timely intervention prevents progression to these severe complications.
Management and Treatment Options
Medical Management
- Indicated for preterm neonates
- Prostaglandin inhibitors such as:
- Indomethacin
- Ibuprofen
- Act by decreasing prostaglandin synthesis, leading to ductal constriction.
Contraindications: Renal insufficiency, bleeding disorders, NEC
Interventional Closure
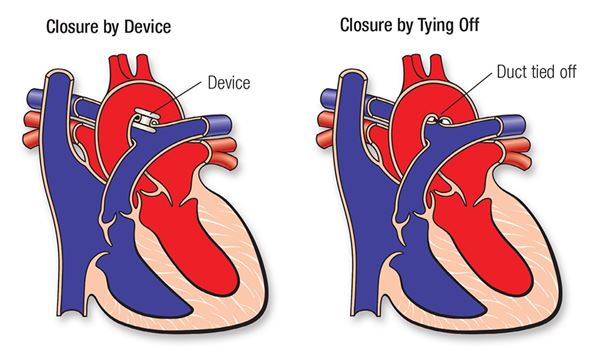
Transcatheter Device Closure:
- Preferred in older infants and children
- Performed via femoral vein access
- Uses coil embolization or Amplatzer duct occluder
- Low complication rates and short hospital stay
Surgical Ligation:
- Indicated when device closure is not feasible
- Performed via thoracotomy
- High success rate but more invasive
Post-Treatment Prognosis and Follow-Up
Prognosis:
- Excellent in treated cases
- Normal life expectancy when closed before pulmonary hypertension develops
Follow-Up:
- Regular echocardiograms post-procedure
- Monitor for residual shunts or stenosis
- Endocarditis prophylaxis for 6 months post device closure
Preventive Strategies
- Antenatal rubella vaccination
- Judicious oxygen therapy in neonates
- Timely screening in preterm infants
- Genetic counseling in syndromic cases
Patent ductus arteriosus remains a common but highly treatable congenital heart defect. Advances in pharmacological and interventional therapy have significantly improved outcomes, particularly in premature infants and neonates. Prompt diagnosis and individualized treatment strategies tailored to ductal size and symptom severity are essential to prevent long-term complications such as pulmonary hypertension or heart failure. Interdisciplinary care involving neonatologists, cardiologists, and cardiothoracic surgeons ensures optimal patient management and prognosis.