Pasteurella multocida osteomyelitis is an uncommon but serious infection of the bone caused by Pasteurella multocida, a facultative anaerobic, Gram-negative coccobacillus. This zoonotic pathogen is part of the normal oral flora of domestic animals, particularly cats and dogs. Human infection usually occurs following bites, scratches, or licks on broken skin, leading to local tissue infection that can advance to deeper structures, including bone.
Osteomyelitis due to P. multocida is particularly concerning due to its rapid onset, aggressive nature, and potential for chronic infection if not promptly and effectively treated.
Pathogenesis and Transmission Pathways
The pathogen typically gains entry through direct inoculation—most commonly through an animal bite or scratch. Following entry, the bacteria can travel via the bloodstream (hematogenous spread) or from contiguous infected soft tissue to the bone.
Epidemiology and Risk Factors
Although Pasteurella species are responsible for a significant proportion of soft tissue infections following animal exposure, osteomyelitis caused by P. multocida remains relatively rare. However, its true incidence may be underestimated due to misidentification or underreporting.
Risk Factors:
- Animal bites (especially from cats due to puncture wounds)
- Immunocompromised status (e.g., diabetes, HIV, cancer therapy)
- Peripheral vascular disease
- Pre-existing bone disease or trauma
- Delayed medical attention after animal injury
Clinical Manifestations
The presentation of Pasteurella multocida osteomyelitis may vary based on the site of infection and the route of bacterial entry.
Common Symptoms:
- Localized bone pain and tenderness
- Swelling and erythema over the affected site
- Restricted range of motion (if joint involvement)
- Fever and systemic signs of infection in advanced stages
- Purulent discharge or sinus tract formation in chronic cases
Common Sites of Involvement:
- Hands and fingers (after cat bites)
- Lower extremities
- Joints adjacent to infected bones (septic arthritis may co-occur)
Diagnostic Evaluation
Accurate and prompt diagnosis is essential for effective management. Clinical history, especially exposure to animals, is crucial.
Microbiological Confirmation:
- Wound and tissue cultures: Identification of P. multocida from aspirates or surgical samples
- Blood cultures: Especially in systemic or chronic cases
- Gram stain: Small Gram-negative rods, oxidase- and catalase-positive
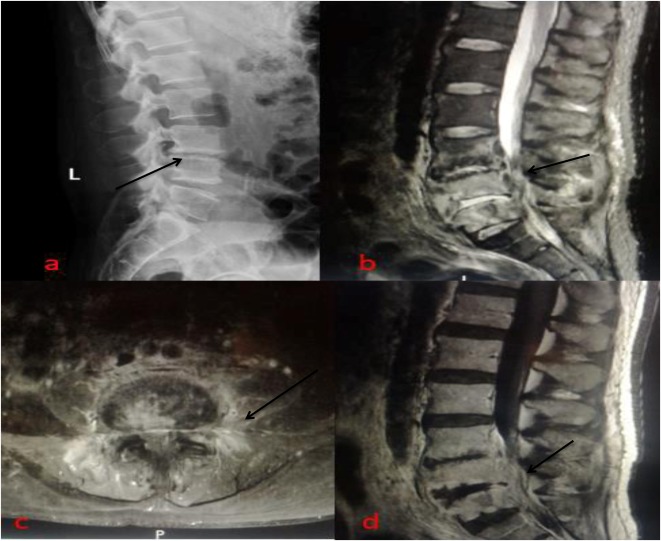
Imaging:
- X-ray: May show bone lysis, periosteal reaction (late findings)
- MRI: Most sensitive for early bone marrow involvement
- CT scan: Useful for evaluating cortical bone integrity and abscesses
Laboratory Studies:
- Elevated white blood cell count, CRP, and ESR
- Consider serological tests in complicated or atypical cases
Antimicrobial Therapy
Prompt initiation of targeted antibiotic therapy is the cornerstone of treatment. P. multocida generally exhibits susceptibility to beta-lactams but is resistant to first-generation cephalosporins and clindamycin.
First-Line Antibiotics:
| Antibiotic | Route | Dosage | Duration |
|---|---|---|---|
| Penicillin G | IV | 18–24 million units/day | 4–6 weeks |
| Ampicillin-Sulbactam | IV | 12 g/day divided | 4–6 weeks |
| Ceftriaxone | IV | 2 g/day | 4–6 weeks |
| Amoxicillin-Clavulanate | Oral (step-down) | 875/125 mg BID | After IV phase |
- Note: Avoid empiric use of macrolides, clindamycin, and first-gen cephalosporins unless sensitivity is confirmed.
Combination Therapy:
- Consider adding gentamicin for synergy in severe cases, especially in immunocompromised patients.
Surgical Intervention
Surgical debridement may be required in patients with:
- Necrotic or devitalized bone
- Abscess formation
- Failure of antibiotic therapy alone
- Chronic osteomyelitis with sinus tract
Surgical Options:
- Debridement and drainage
- Sequestrectomy
- Bone grafting or reconstruction in advanced cases
Prognosis and Long-Term Outcomes
With early and appropriate therapy, the prognosis is favorable. However, delayed diagnosis or inadequate treatment increases the risk of chronic osteomyelitis and permanent structural damage.
Prognostic Factors:
- Time to diagnosis
- Host immune status
- Adequacy of surgical intervention
- Duration and appropriateness of antibiotics
Prevention and Public Health Considerations
Given the zoonotic nature of P. multocida, prevention strategies are centered around responsible animal interactions and wound care.
Preventive Measures:
- Avoiding rough play with pets that may lead to bites or scratches
- Immediate wound irrigation and antiseptic application after animal contact
- Prophylactic antibiotics in high-risk wounds (e.g., puncture wounds from cats)
- Public awareness regarding risks of untreated animal bites
Pasteurella multocida osteomyelitis, though rare, is a clinically significant infection necessitating a high index of suspicion, particularly following animal exposure. Early microbiological diagnosis, guided antimicrobial therapy, and surgical management when needed are essential for favorable outcomes. Multidisciplinary collaboration between infectious disease specialists, orthopedic surgeons, and primary care providers ensures optimal patient recovery and minimizes long-term complications.