Pasteurella multocida endocarditis represents a rare but increasingly recognized form of zoonotic infective endocarditis. This Gram-negative, facultatively anaerobic coccobacillus is commonly found in the oropharyngeal flora of domestic animals, especially cats and dogs. Human infections typically follow animal bites, scratches, or close contact. Though commonly associated with soft tissue infections, Pasteurella multocida can invade deeper tissues, including cardiac valves, leading to endocarditis—a life-threatening condition requiring prompt diagnosis and targeted treatment.
Epidemiology and Transmission Pathways
Pasteurella multocida endocarditis remains uncommon, with limited cases reported in medical literature. However, the condition’s incidence may be underdiagnosed due to its rarity and often non-specific presentation.
- Primary Source: Animal exposure (cat or dog bites, scratches, or licks over open wounds)
- Predisposing Factors: Pre-existing valvular disease, prosthetic heart valves, immunosuppression, chronic illnesses (e.g., diabetes, cirrhosis)
Clinical Presentation of Pasteurella Endocarditis
The signs and symptoms are similar to those observed in classic infective endocarditis, though often with a rapid onset and aggressive course due to Pasteurella’s virulence.
Common Clinical Features:
- Fever and chills
- Heart murmur or worsening of pre-existing murmur
- Fatigue and malaise
- Splenomegaly
- Peripheral signs: Petechiae, Janeway lesions, Osler nodes (less common)
Complications:
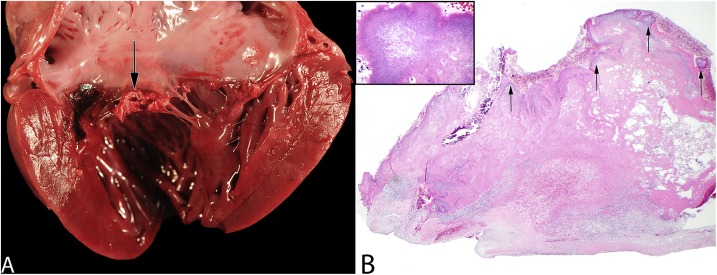
- Valvular destruction
- Congestive heart failure
- Embolic phenomena (stroke, renal infarction, septic emboli)
- Septicemia and multiorgan failure
Diagnostic Workup for Pasteurella multocida Endocarditis
Blood Cultures
- Key Diagnostic Tool: Pasteurella multocida is usually detected in multiple blood cultures.
- Time to positivity: Typically within 24–48 hours
- Culture Characteristics: Oxidase-positive, catalase-positive, sensitive to penicillin
Echocardiography
- Transthoracic (TTE): Initial evaluation
- Transesophageal (TEE): Superior sensitivity for detecting vegetations, abscesses, and prosthetic valve involvement
Additional Tests
- CBC: Leukocytosis may be present
- Inflammatory markers: Elevated CRP and ESR
- Imaging: Chest X-ray or CT if embolic complications are suspected
Pathophysiology and Virulence Factors
Pasteurella multocida exhibits several mechanisms facilitating endocardial colonization:
- Capsular polysaccharides: Protect against phagocytosis
- Lipopolysaccharides (LPS): Induce strong inflammatory response
- Iron acquisition systems: Aid survival in bloodstream
- Adhesion proteins: Enable colonization of damaged endothelium or prosthetic material
These features contribute to rapid progression and aggressive valve destruction.
Treatment and Management of Pasteurella Endocarditis
Antimicrobial Therapy
Early and appropriate antibiotic therapy is critical. Most strains are susceptible to β-lactam antibiotics.
| Antibiotic | Dosage | Duration | Notes |
|---|---|---|---|
| Penicillin G | 18–24 million units/day IV | 4–6 weeks | First-line |
| Ceftriaxone | 2 g/day IV | 4–6 weeks | Alternative if penicillin allergy |
| Ampicillin-Sulbactam | 12 g/day IV | 4–6 weeks | Broader coverage |
| Gentamicin | 3 mg/kg/day IV | 2 weeks (with β-lactam) | Synergy in some cases |
- Note: Resistance to macrolides, aminoglycosides, and tetracyclines may occur; susceptibility testing is advised.
Surgical Intervention
Valve surgery may be indicated in:
- Heart failure due to valvular dysfunction
- Large vegetations (>10 mm)
- Persistent bacteremia despite antibiotics
- Prosthetic valve involvement
- Recurrent embolization
Prognosis and Outcomes
Early detection and targeted therapy often lead to favorable outcomes. However, delayed treatment or inappropriate antibiotic use can result in high morbidity and mortality.
Factors Affecting Prognosis:
- Time to diagnosis
- Prompt initiation of effective antibiotics
- Underlying comorbidities
- Need for surgical intervention
Mortality rates range from 15% to 30%, often linked to complications or delayed management.
Prevention and Risk Mitigation
Key Preventive Strategies:
- Animal bite care: Immediate wound cleaning and prophylactic antibiotics for high-risk patients
- Public education: Awareness about zoonotic infections from pets
- Monitoring in high-risk individuals: Especially those with prosthetic valves or immunosuppression
- Veterinary health of companion animals: Regular pet checkups and hygiene
Pasteurella multocida endocarditis is a rare but serious condition requiring heightened clinical suspicion, especially in patients with recent animal exposure and underlying cardiac conditions. Comprehensive diagnostic evaluation, rapid initiation of appropriate antibiotics, and timely surgical intervention when indicated are paramount for successful outcomes. Collaborative efforts between infectious disease specialists, cardiologists, and surgeons play a vital role in managing this challenging zoonotic endocarditis.